AVNRT – Important Points
• No P waves ( Can be Inverted In II,III, aVF)
• Narrow QRS Tachycardia
• Regular R-R Interval
• Atypical AVNRT – Psudo r waves
• Rx – Vagal maneuvers, Valsalva, Diving Reflex
• Drugs – ABCD Of AVNRT
- A- Adenosine
- B- Beta Blockers (eg. Metoprolol)
- C- Calcium Channel Blockers (eg. Verapamil)
- D – Digoxin
• If patient is on Theophylline – Higher Doses of adenosine are required
• Vitally Unstable – Electrical Cardioversion
Overview:
Atrioventricular nodal reentrant tachycardia (AVNRT) is a most common supraventricular arrhythmia characterized by rapid heart rates originating within the atrioventricular (AV) node. Although, SVT includes any tachycardia that originate from above the ventricles, AVNRT is most commonly reffered as SVT.
Causes of AVNRT:
- Electrical Circuitry Abnormalities:
- AVNRT arises from abnormal pathways within the AV node, facilitating reentrant circuits.
- These pathways create a loop of electrical signals, leading to rapid and regular tachycardia.
- Triggering Factors:
- Various factors such as stress, caffeine, nicotine, and certain medications can precipitate AVNRT episodes.
- These triggers disrupt the delicate balance of electrical impulses within the AV node, leading to arrhythmia onset.
Symptoms of AVNRT:
- Palpitations:
- Sudden awareness of rapid, pounding, or irregular heartbeat is a hallmark symptom.
- Patients often describe a sensation of fluttering or racing within the chest.
- Dizziness and Syncope:
- Decreased cerebral perfusion due to rapid heart rate can manifest as dizziness or lightheadedness.
- In severe cases, syncope or near-syncope may occur, particularly with prolonged episodes.
- Chest Discomfort:
- Some individuals may experience chest tightness or discomfort resembling angina pectoris.
- This sensation is often secondary to increased myocardial oxygen demand during tachycardia.
- Anxiety and Sweating:
- The adrenaline surge accompanying AVNRT can induce feelings of anxiety or impending doom.
- Sweating and other autonomic symptoms may accompany the arrhythmic episode.
ECG Changes :
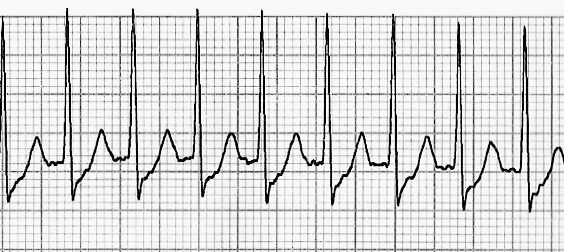
- Narrow QRS Complexes:
- QRS duration typically measures less than 0.12 seconds, indicating a supraventricular origin.
- The narrow QRS complexes differentiate AVNRT from ventricular tachycardia.
- Regular Rhythm:
- AVNRT typically exhibits a regular rhythm, with consistent RR intervals throughout the ECG tracing.
- This regularity reflects the stable reentrant circuitry within the AV node.
- Absence of P Waves:
- P waves may be absent or obscured within the QRS complexes or follow them closely.
- This phenomenon, known as “hidden P waves,” is characteristic of AVNRT.
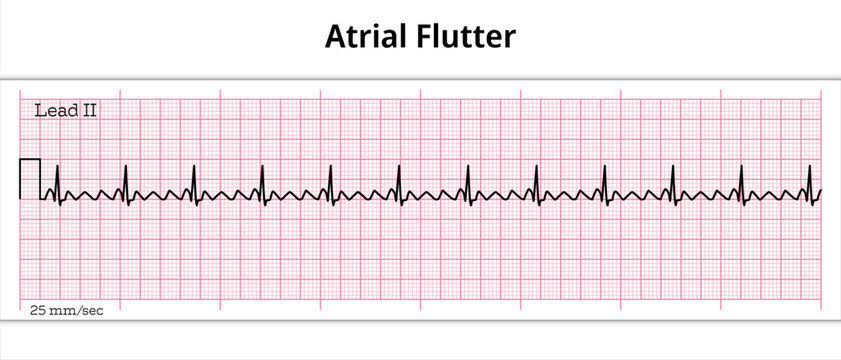
SVT vs. VT ECG Changes Difference:
- P-Wave Morphology:
- In AVNRT, P waves may be absent, hidden, or closely associated with QRS complexes.
- Ventricular tachycardia (VT) often displays dissociated P waves unrelated to QRS complexes.
- QRS Complex Width:
- SVT, including AVNRT, typically presents with narrow QRS complexes (<0.12 sec).
- In contrast, VT exhibits wide QRS complexes (>0.12 sec) due to ventricular origin.
- Clinical Context:
- AVNRT predominantly occurs in patients without underlying structural heart disease.
- VT is commonly associated with structural heart abnormalities or prior myocardial infarction.
Treatment of AVNRT:
- Vagal Maneuvers:
- Techniques such as the Valsalva maneuver or carotid sinus massage stimulate the vagus nerve, potentially terminating AVNRT.
- These maneuvers increase vagal tone, slowing conduction through the AV node and disrupting reentrant circuits.
- Adenosine Administration:
- Rapid intravenous administration of adenosine can transiently block AV nodal conduction, terminating AVNRT.
- Adenosine induces a transient pause in cardiac activity, allowing the reentrant circuitry to reset.
- Calcium Channel Blockers or Beta-Blockers:
- Verapamil or metoprolol may be administered intravenously for acute termination of AVNRT episodes.
- These medications exert negative chronotropic and dromotropic effects, slowing AV nodal conduction and terminating tachycardia.
- Radiofrequency Catheter Ablation:
- Curative treatment for AVNRT involves catheter-based ablation of the abnormal AV nodal pathways.
- Radiofrequency energy is delivered via a catheter to selectively destroy the tissue responsible for reentrant circuits.
Complications:
- Syncope and Hemodynamic Instability:
- Persistent AVNRT episodes can lead to decreased cardiac output, causing syncope or hemodynamic instability.
- Prompt recognition and intervention are crucial to prevent adverse outcomes.
- Stroke and Thromboembolism:
- Although rare, thrombus formation within the atria may occur during prolonged AVNRT episodes, leading to embolic events.
- Thromboembolic prophylaxis may be necessary in high-risk patients.
- Arrhythmia Progression:
- Untreated or recurrent AVNRT episodes may increase the risk of developing atrial fibrillation or other arrhythmias.
- Long-term management and follow-up are essential to monitor for arrhythmia recurrence and progression.
AVNRT is a common and treatable supraventricular arrhythmia characterized by rapid heart rates originating within the AV node.
Pingback: Meningitis - Causes, Symptoms, Treatment - Modern Health
Pingback: Uses of Atropine - Dose & Routes - Modern Health
Pingback: Toxic Megacolon - Causes , Treatment - Modern Health