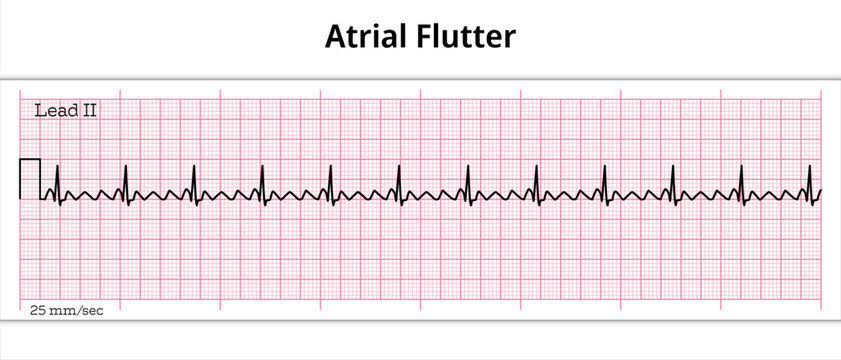
Atrial flutter – Important ECG Changes:
- Regular ventricular response
- Sawtooth pattern on ECG
- Atrial rate to ventricular rate ratio can vary (2:1, 3:1, etc.)
- Atrial rate typically between 250 to 350 beats per minute
Atrial flutter is a cardiac arrhythmia (Supraventricular Origin) characterized by rapid and regular atrial contractions.
What is Atrial Flutter?
Atrial flutter is a type of abnormal heart rhythm that originates in the atria, the upper chambers of the heart. Instead of the normal sinus rhythm, where the atria contract in a coordinated manner, atrial flutter involves rapid contractions, typically at rates between 250 to 350 beats per minute.
Rhythm:
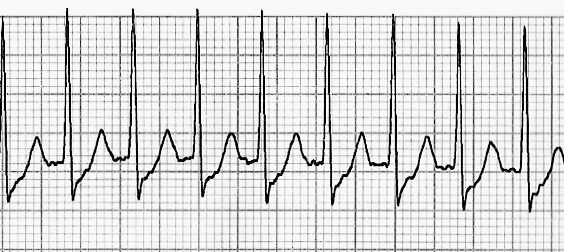
In atrial flutter, the electrical impulses in the heart’s atria circulate rapidly around specific areas, creating a characteristic “sawtooth” pattern on an electrocardiogram (ECG). This pattern, known as “F waves” or “flutter waves,” indicates the irregular electrical activity in the atria.
Symptoms:
The symptoms of atrial flutter can vary from person to person but often include
- palpitations
- shortness of breath
- chest discomfort
- Fatigue
- Dizziness.
- Fainting or syncope (Severe Cases)
ECG Changes in Atrial Flutter:
The characteristic ECG changes associated with this arrhythmia include:
- Sawtooth Pattern (F Waves): A hallmark of atrial flutter, F waves appear as rapid, regular, and uniform oscillations on the ECG tracing. These waves represent atrial depolarizations occurring at a rate typically between 250 to 350 beats per minute.
- Regular Ventricular Response: Despite the rapid atrial activity, the ventricular response in atrial flutter is usually regular, maintaining a consistent heart rate.
- Atrial Rate: The atrial rate in atrial flutter typically ranges between 250 to 350 beats per minute, contributing to the characteristic rapid atrial contractions seen on the ECG.
- Atrial Rate to Ventricular Rate Ratio: The relationship between the atrial and ventricular rates can vary, often presenting as a 2:1, 3:1, or other ratios, depending on the conduction properties of the atrioventricular node.
- Flutter Waves Alignment: Flutter waves on the ECG tracing typically exhibit a consistent alignment, giving rise to the appearance of a sawtooth pattern. This regularity distinguishes atrial flutter from other arrhythmias.
- Absence of P Waves: In some cases, P waves may be absent or obscured within the flutter waves due to the rapid atrial activity, making it challenging to discern individual atrial depolarizations.
- Narrow QRS Complexes: The QRS complexes on the ECG tracing remain narrow, indicating normal ventricular depolarization and conduction despite the underlying atrial arrhythmia.
- ST Segment and T Wave Changes: In some cases, atrial flutter may lead to subtle ST segment or T wave abnormalities, reflecting myocardial ischemia or altered ventricular repolarization secondary to the arrhythmia.
Causes:
Atrial flutter can be triggered by various factors, including:
- Heart Disease: Conditions such as coronary artery disease, hypertension, and cardiomyopathy can increase the risk of atrial flutter.
- Electrolyte Imbalance: Abnormal levels of electrolytes, such as potassium or magnesium, can disrupt the heart’s electrical activity and contribute to arrhythmias.
- Thyroid Disorders: Thyroid imbalances, particularly hyperthyroidism, can predispose individuals to atrial flutter.
- Previous Heart Surgery: Patients who have undergone cardiac procedures, such as valve surgery or coronary artery bypass grafting, may be at higher risk.
- Stimulants: Excessive consumption of stimulants like caffeine or certain medications can trigger atrial flutter episodes.
Treatment of Atrial Flutter:
Treatment strategies for atrial flutter aim to control symptoms, prevent complications, and restore normal heart rhythm. Depending on the patient’s condition and medical history, treatment options may include:
- Medications: Antiarrhythmic drugs, such as flecainide, propafenone, or amiodarone, may be prescribed to help regulate the heart’s electrical activity and maintain normal sinus rhythm.
- Cardioversion: Electrical cardioversion involves delivering a controlled electric shock to the heart to reset its rhythm to normal.
- Catheter Ablation: During this minimally invasive procedure, a catheter is inserted into the heart to destroy the abnormal electrical pathways responsible for atrial flutter.
- Rate Control: In some cases, the focus may be on controlling the heart rate rather than restoring normal sinus rhythm, especially in individuals with persistent atrial flutter.
- Anticoagulation: Since atrial flutter increases the risk of blood clots and stroke, anticoagulant medications like warfarin or direct oral anticoagulants (DOACs) may be prescribed to reduce this risk.
Complications:
If left untreated or poorly managed, atrial flutter can lead to several complications, including:
- Cradio-Embolic Stroke: Blood clots can form in the atria due to stagnant blood flow, increasing the risk of stroke if a clot travels to the brain.
- Heart Failure: Prolonged episodes of atrial flutter can weaken the heart muscle and impair its ability to pump blood effectively.
- Recurrent Arrhythmias: Atrial flutter may recur, especially if underlying risk factors are not addressed or if treatment is ineffective.
- Cardiovascular Events: Atrial flutter can contribute to other cardiovascular events such as myocardial infarction (heart attack) or pulmonary embolism (blood clot in the lungs).
In conclusion, atrial flutter is a common cardiac arrhythmia that requires prompt diagnosis and appropriate management to prevent complications and improve outcomes. With a comprehensive understanding of its causes, symptoms, and treatment options, healthcare providers can effectively guide patients towards optimal heart health.
Pingback: common health conditions - MedTimes
Pingback: Common health conditions - MedWebMD