Meningitis;
Important points:
Common Causes:
- Streptococcus pneumoniae
- Neisseria meningitidis
- Haemophilus influenzae type b (Hib)
- Group B Streptococcus (in neonates)
- Enteroviruses
- Herpes simplex virus (HSV)
- Varicella-zoster virus (VZV)
- Human herpesvirus 6 (HHV-6)
- Epstein-Barr virus (EBV)
- Cryptococcus neoformans
- Candida species
- Naegleria fowleri (primary amoebic meningoencephalitis, rare)
Signs and Examination Findings:
- Kernig’s Sign: Inability to fully extend the knee with hip flexion while the individual is lying supine.
- Brudzinski’s Sign: Flexion of the hips and knees in response to passive neck flexion.
- Nuchal Rigidity: Stiffness and pain in the neck when attempting to flex the neck forward.
- Positive Babinski Sign: Dorsiflexion of the big toe and fanning of the other toes when the sole of the foot is stroked.
- Photophobia: Sensitivity to light, causing discomfort or pain when exposed to light.
- Altered Mental Status: Confusion, irritability, lethargy, or coma.
Overview:
Meningitis, an inflammation of the protective membranes covering the brain and spinal cord, poses a significant health threat worldwide. Timely recognition and management are paramount to prevent severe complications and reduce mortality rates associated with this condition.
Symptoms of Meningitis:
The presentation of meningitis can vary depending on the causative agent and the age of the affected individual. Common symptoms and signs include:
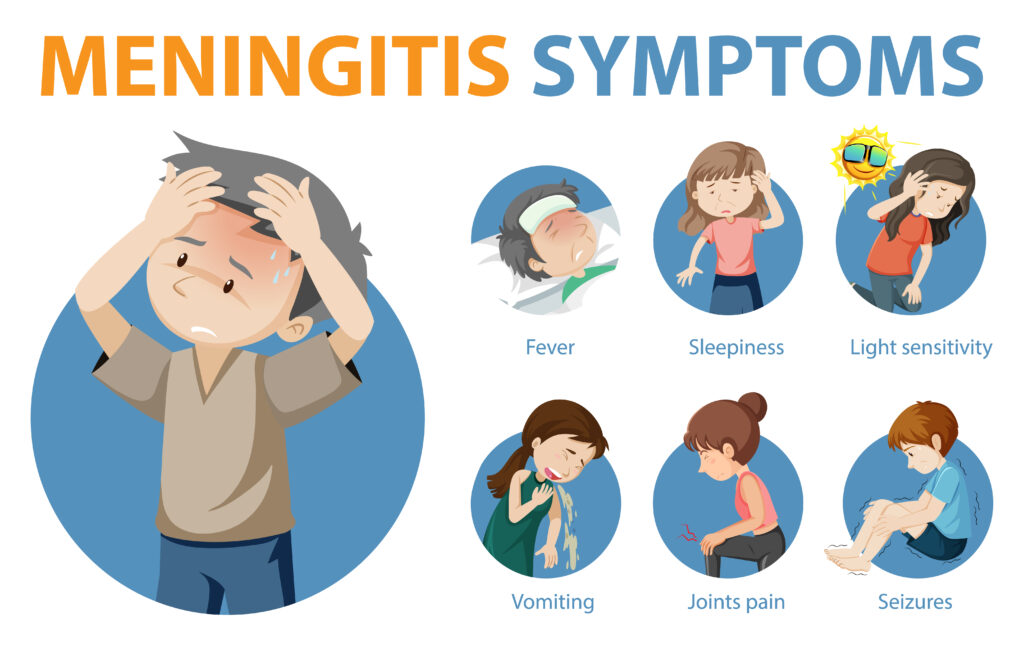
- Headache: Persistent and severe headache is a hallmark symptom of meningitis.
- Fever: High fever is often present and may be accompanied by chills and rigors.
- Stiff Neck: Neck stiffness, especially when trying to touch the chin to the chest, is characteristic.
- Photophobia: Sensitivity to light is common, along with other neurological symptoms such as confusion or altered mental status.
- Nausea and Vomiting: Gastrointestinal symptoms may be present, particularly in children.
- Rash: Meningococcal meningitis can cause a characteristic purpuric rash that does not blanch with pressure.
Causes of Meningitis:
- Bacterial Meningitis:
- Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae are common bacterial pathogens.
- Bacterial meningitis is often more severe and can progress rapidly without treatment.
- Viral Meningitis:
- Enteroviruses, herpesviruses, and adenoviruses are common viral causes.
- Viral meningitis is typically less severe than bacterial meningitis and often resolves without specific treatment.
- Fungal Meningitis:
- Cryptococcus neoformans and Histoplasma capsulatum are common fungal pathogens.
- Fungal meningitis is more common in immunocompromised individuals and may require prolonged treatment.
Clinical Examination in Meningitis:
1. Neurological Assessment:
- Mental Status: Evaluate for altered mental status, confusion, or decreased level of consciousness.
- Cranial Nerves: Assess cranial nerve function, including extraocular movements, facial sensation and symmetry, and gag reflex.
- Motor and Sensory Function: Test muscle strength, tone, and sensation in all extremities.
- Reflexes: Check deep tendon reflexes such as the biceps, triceps, and patellar reflexes for abnormalities.
2. Evaluation of Meningeal Irritation:
- Neck Stiffness: Have the patient attempt to touch their chin to their chest to assess for resistance or discomfort.
- Kernig’s Sign: Flex the patient’s hip and knee to 90 degrees while lying flat, then attempt to straighten the knee. Pain or resistance indicates a positive sign.
- Brudzinski’s Sign: Flex the patient’s neck, and observe for involuntary flexion of the hips and knees. Positive sign suggests meningeal irritation.
3. Assessment of Vital Signs:
- Temperature: Measure body temperature for fever, a common sign of meningitis.
- Heart Rate: Monitor heart rate for signs of tachycardia, which may indicate systemic infection or hemodynamic instability.
- Blood Pressure: Check blood pressure for signs of hypotension or shock, particularly in severe cases of meningitis.
- Respiratory Rate: Assess respiratory rate for signs of respiratory distress or compromise.
4. Skin Examination:
- Rash: Look for a characteristic purpuric rash that does not blanch with pressure, which may suggest meningococcal meningitis.
- Petechiae: Check for tiny, pinpoint red or purple spots on the skin, mucous membranes, or conjunctiva, which may indicate septicemia.
5. Fundoscopic Examination:
- Papilledema: Look for optic disc swelling, which may suggest increased intracranial pressure secondary to meningitis.
- Retinal Hemorrhages: Examine for retinal hemorrhages, which may be present in severe cases of meningococcal meningitis or disseminated intravascular coagulation.
6. Assessment of Systemic Manifestations:
- Respiratory System: Listen for abnormal breath sounds such as crackles or diminished breath sounds, which may indicate associated pneumonia.
- Cardiovascular System: Check for signs of tachycardia, hypotension, or signs of shock, which may indicate systemic involvement or sepsis.
- Gastrointestinal System: Assess for nausea, vomiting, or abdominal pain, which may accompany meningitis, particularly in children.
7. Evaluation of Fontanelle (in infants):
- Bulging Fontanelle: Palpate the infant’s fontanelle for bulging, which may indicate increased intracranial pressure associated with meningitis.
- Sunken Fontanelle: Conversely, a sunken fontanelle may suggest dehydration, which can complicate meningitis in infants.
Laboratory Diagnosis of Meningitis:
- Lumbar Puncture:
- Cerebrospinal fluid (CSF) analysis is crucial for diagnosing meningitis.
- CSF findings typically include elevated white blood cell count, elevated protein levels, and decreased glucose levels.
• CSF findings in bacterial, viral, and tuberculous meningitis :
| CSF Finding | Bacterial Meningitis | Viral Meningitis | Tuberculous Meningitis |
|---|---|---|---|
| Appearance | Cloudy or turbid | Clear or slightly cloudy | Clear or slightly cloudy |
| Cell Count (WBC) | Elevated, >1000 cells/mm³, predominantly neutrophils | Mild to moderately elevated, <1000 cells/mm³, predominantly lymphocytes | Moderately elevated, predominantly lymphocytes and monocytes |
| Glucose Level | Decreased, <40 mg/dL | Normal | Decreased, similar to bacterial meningitis |
| Protein Level | Elevated, >100 mg/dL | Slightly elevated, typically <100 mg/dL | Elevated, >100 mg/dL |
| Gram Stain | Positive for bacteria | Not applicable | Not applicable |
| PCR Testing | Not applicable | Positive for viral DNA/RNA | Not applicable |
| ADA Activity | Not applicable | Not applicable | Elevated, supporting diagnosis |
.
- Microbiological Testing:
- Gram stain and culture of CSF help identify the causative organism, guiding appropriate antimicrobial therapy.
- Polymerase chain reaction (PCR) testing can rapidly detect viral or bacterial DNA in CSF samples.
Treatment:
Drugs and Doses for Meningitis Treatment
1. Antibiotics for Bacterial Meningitis:
- Empirical Therapy:
- Ceftriaxone: 2 grams IV every 12 hours OR
- Cefotaxime: 2 grams IV every 4-6 hours OR
- Meropenem: 2 grams IV every 8 hours
- Consider adding Vancomycin: 15 mg/kg IV every 6-8 hours for empiric coverage of resistant Streptococcus pneumoniae or suspected methicillin-resistant Staphylococcus aureus (MRSA) infection.
- Definitive Therapy (Based on Culture and Sensitivity):
- Adjust antibiotics based on culture results and susceptibilities.
2. Antiviral Agents for Viral Meningitis:
- Acyclovir:
- Adult Dose: 10-15 mg/kg IV every 8 hours for 10-14 days.
- Pediatric Dose: 20 mg/kg IV every 8 hours for 10-14 days.
- Duration may vary based on the severity of the infection and clinical response.
3. Antituberculous Therapy for Tuberculous Meningitis:
- First-Line Agents:
- Isoniazid (INH): 5 mg/kg/day orally (maximum 300 mg/day).
- Rifampin: 10 mg/kg/day orally (maximum 600 mg/day).
- Pyrazinamide: 25-30 mg/kg/day orally (maximum 2 grams/day).
- Ethambutol: 15-20 mg/kg/day orally (maximum 1.2 grams/day).
- Adjunctive Therapy:
- Prednisone: 1-2 mg/kg/day orally for 4-8 weeks, followed by gradual tapering.
- Consideration of additional agents such as Streptomycin or Amikacin in severe cases or drug-resistant TB.
4. Adjunctive Therapy:
- Dexamethasone:
- Adult Dose: 10 mg IV every 6 hours for 2-4 days, then 4 mg IV every 6 hours for 2-4 days.
- Pediatric Dose: 0.15 mg/kg IV every 6 hours for 2-4 days, then 0.1 mg/kg IV every 6 hours for 2-4 days.
- Administer before or concomitantly with the first dose of antibiotics in bacterial meningitis to reduce the risk of neurological complications and mortality.
- Maintenance Fluids:
- Ensure adequate hydration with intravenous fluids to prevent dehydration and maintain electrolyte balance.
5. Supportive Care:
- Analgesics:
- Use acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) for headache and fever control.
- Antipyretics:
- Administer antipyretics such as acetaminophen to reduce fever and alleviate discomfort.
- Antiemetics:
- Consider antiemetic agents for nausea and vomiting.
- Monitoring and Surveillance:
- Regular monitoring of vital signs, neurological status, and response to treatment is essential for guiding management and detecting complications.
6. Duration of Treatment:
- Bacterial Meningitis:
- Antibiotic therapy typically continues for 10-14 days or longer based on clinical response and CSF parameters.
- Viral Meningitis:
- Antiviral therapy with acyclovir is usually administered for 10-14 days or longer as needed.
- Tuberculous Meningitis:
- Antituberculous therapy is prolonged, often for 9-12 months or more, depending on the severity of the infection and the patient’s clinical response.
Summary:
Meningitis remains a significant public health concern, with bacterial meningitis posing the greatest risk of morbidity and mortality.


Pingback: Neurocystecercosis - Causes, Symptoms, Treatment - Modern Health