Type 2 Diabetes Mellitus;
Quick Facts:
- Insulin Resistance present
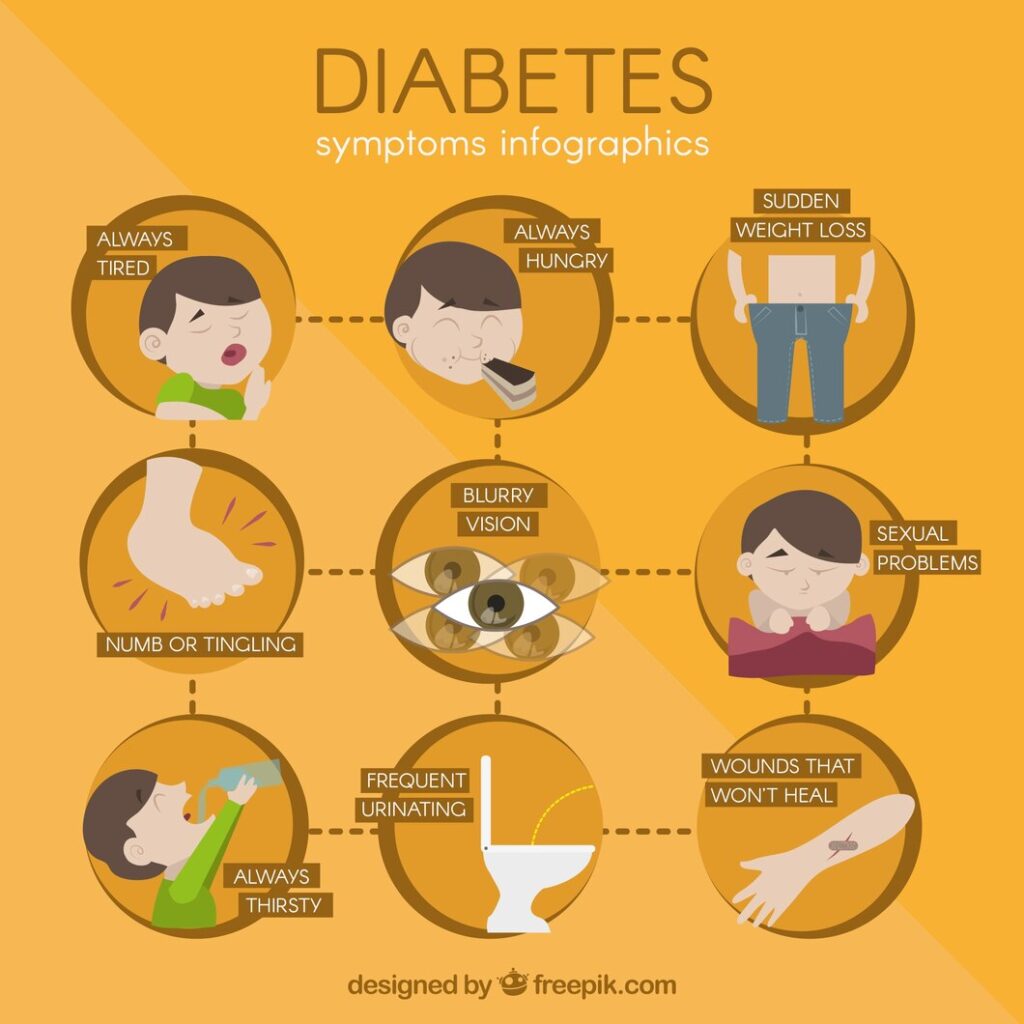
- Symptoms – Frequent Micturition, Weight loss, blurred vision, Recurrent UTIs, Tingling, Hungry
- Rx – Metformin, Diet, Weight management, Exercises
- Retinopathy (Vision Loss), Neuropathy (Tingling etc), Nephropathy (Kidney Damage), Diabetic foot etc are complications
- HbA1C aim less than 7
Overview:
Type 2 Diabetes Mellitus is an endocrine disorder in which body cannot control blood sugar levels and that is mainly because of insulin resistance. This is very common and very burdensome condition which can be managed very nicely with medications with other lifestyle modifications.
What is type 2 Diabetes Mellitus?
Type 2 diabetes is a chronic endocrine disorder in which our body cannot control blood sugar levels. The main reason for this is insulin resistance. Insulin resistance is a condition in which body makes enough insulin, but cannot respond to it. That’s why insulin is almost of no use or is less effective.
What is Insulin Resistance?
Insulin resistance is a term that tells us that our body is not responding to insulin at the levels it supposed to respond. This leads to rise in blood glucose levels and Diabetes. Insulin is normally required by our body cells to take glucose from blood.
If insulin is absent or is less effective then our body cells cannot take glucose from blood. This leads to accumulation of glucose in blood itself and leads to hyperglycemia (High Blood sugar). Despite of high blood glucose levels, cells don’t have Glucose, which is a fuel for our cells.
On one hand there is high blood sugar (Glucose) levels, while on other hand our body cells still have low glucose inside them available to use as a fuel.
Signs and symptoms of Type 2 DM:
Type 2 DM is a condition which takes years to show itself truly. We must keep watch on minor signs and symptoms that we keep ignoring for years before this condition starts to show it’s complications. Let’s see what are common signs and symptoms:
- Always Hungry – Type 2 DM patient have a high hunger, they keep getting hungry despite of eating several times a day. This is because our body thinks that our cells are starving because they don’t have Glucose, so our body tries to elevate blood sugar levels by all means available.
- Frequent Micturition / Peeing – Our kidneys throw out the excess levels of glucose from blood into urine. In order to throw that excess glucose, more water is thrown out into urine, and thats why these patients have to pee more often.
- Weight loss – Due to inability to use glucose, our cells starv and this signals by our body. So in order to make glucose available to these starving cells, our body try to produce glucose from fat stored in our body and also from our muscles (Protein Breakdown). This all results in weight loss.
- Recurrent Urinary Infections (UTIs) – There is high glucose in urine of patients with Diabetes. This is a favourable environment for pathogenic microbes to grow. That’s why these patients have recurrent Urinary track infections.
- Non Healing wounds – If someone has a wound and it’s not healing despite of taking all necessary precautions, medications and wound care, then it’s time to get your blood sugar levels checked. Patients with DM have blocked blood vessels and poor blood supply. This leads to non Healing of wounds.
- Tingling sensations / Parasthesias – Uncontrolled diabetes can involve nerves and cause neuropathy. This csn manifests commonly as tingling sensations.
- Blurred vision – This is often a late symptom when uncontrolled diabetes involves eyes and cause retinopathy.
How to diagnose Type 2 DM?
After taking a brief history if you are suspecting that a person might be having Diabetes then first of all we must check his/her blood sugar levels.
1. Blood Tests:
- Fasting Plasma Glucose (FPG) Test: This test measures blood sugar levels after fasting for at least eight hours. A fasting plasma glucose level of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions indicates diabetes.
- Random Plasma Glucose Test: Blood glucose levels are measured at any time of the day, irrespective of the last meal. A random plasma glucose level of 200 mg/dL or higher, along with classic symptoms of diabetes, may indicate the presence of the condition.
- Oral Glucose Tolerance Test (OGTT): This test involves measuring blood sugar levels before and two hours after consuming a sugary drink. A blood glucose level of 200 mg/dL or higher two hours after ingesting the glucose solution confirms diabetes.
- Hemoglobin A1c (HbA1c) Test: The HbA1c test measures the average blood sugar levels over the past two to three months. An HbA1c level of 6.5% or higher is indicative of diabetes.
2. Screening for Complications at Diagnosis:
- Retinopathy Screening: Dilated eye examination by an ophthalmologist or optometrist is recommended at the time of diabetes diagnosis and annually thereafter to assess for diabetic retinopathy, a leading cause of blindness.
- Neuropathy Screening: Evaluation for peripheral neuropathy should be performed using clinical assessment tools such as monofilament testing, vibration perception threshold testing, or nerve conduction studies.
- Nephropathy Screening: Screening for kidney disease involves assessing urinary albumin excretion and estimating glomerular filtration rate (eGFR) using laboratory tests. Urine albumin-to-creatinine ratio (UACR) and serum creatinine levels are commonly measured.
- Cardiovascular Risk Assessment: Individuals with Type 2 DM are at increased risk of cardiovascular disease. Screening for cardiovascular risk factors such as hypertension, dyslipidemia, and obesity is essential at the time of diagnosis and regularly thereafter.
- Foot Examination: Comprehensive foot examination, including assessment of foot sensation, pulses, and skin integrity, should be conducted to detect peripheral neuropathy and assess the risk of foot ulcers and amputations.
Risk Factors :
Risk factors associated with Type 2 Diabetes Mellitus:
- Family History: Having a close family member with Type 2 DM increases the risk of developing the condition.
- Obesity: Excess body weight, particularly abdominal obesity, is a significant risk factor for insulin resistance and Type 2 DM.
- Sedentary Lifestyle: Lack of physical activity and prolonged sitting increase the risk of developing insulin resistance and Type 2 DM.
- Unhealthy Diet: Consuming a diet high in refined sugars, carbohydrates, and saturated fats, and low in fiber and whole grains increases the risk of Type 2 DM.
- Age: The risk of Type 2 DM increases with age, particularly after 45 years old.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanics, Native Americans, and Asian Americans, have a higher predisposition to Type 2 DM.
- Gestational Diabetes: Women who had gestational diabetes during pregnancy are at increased risk of developing Type 2 DM later in life.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS have a higher risk of insulin resistance and Type 2 DM.
- Hypertension (High Blood Pressure): Having high blood pressure increases the risk of developing Type 2 DM.
- Dyslipidemia (Abnormal Cholesterol Levels): Abnormal levels of cholesterol and triglycerides in the blood are associated with an increased risk of Type 2 DM.
- History of Cardiovascular Disease: Individuals with a history of heart disease or stroke are at higher risk of developing Type 2 DM.
- Sleep Disorders: Conditions such as obstructive sleep apnea are associated with insulin resistance and an increased risk of Type 2 DM.
- Smoking: Smoking increases the risk of Type 2 DM and complicates its management by worsening insulin resistance.
- Stress: Chronic stress and depression may contribute to insulin resistance and increase the risk of Type 2 DM.
- Medications: Certain medications, such as corticosteroids and antipsychotic drugs, can increase the risk of developing Type 2 DM.
Treatment of Type 2 Diabetes Mellitus:
Managing Type 2 Diabetes Mellitus (DM) involves a multifaceted approach aimed at controlling blood sugar levels, preventing complications, and improving overall health and well-being. Treatment strategies typically include lifestyle modifications, medications, and, in some cases, insulin therapy. Let’s see :
1. Lifestyle Modifications:
- Healthy Diet: Emphasizing a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting refined sugars and carbohydrates is essential for managing blood sugar levels. Portion control and meal timing also play crucial roles in glucose control.
- Regular Exercise: Engaging in regular physical activity, such as brisk walking, cycling, or swimming, for at least 150 minutes per week improves insulin sensitivity, helps lower blood sugar levels, and promotes weight management.
- Weight Management: Achieving and maintaining a healthy weight through a combination of diet and exercise is important for reducing insulin resistance and improving blood sugar control in individuals with Type 2 DM.
- Smoking Cessation: Quitting smoking is essential for managing Type 2 DM, as smoking worsens insulin resistance and increases the risk of cardiovascular complications.
- Stress Management: Adopting stress-reduction techniques such as mindfulness, meditation, and relaxation exercises can help improve blood sugar control and overall well-being.
2. Medications:
- Oral Antidiabetic Medications: Several classes of oral medications are available to lower blood sugar levels in individuals with Type 2 DM. These include:
- Metformin: Improves insulin sensitivity and decreases glucose production by the liver.
- Sulfonylureas: Stimulate insulin secretion from the pancreas.
- DPP-4 Inhibitors: Increase insulin secretion and decrease glucagon production.
- GLP-1 Receptor Agonists: Stimulate insulin secretion and decrease appetite.
- SGLT2 Inhibitors: Increase glucose excretion in the urine.
- Injectable Medications: For individuals who do not achieve adequate blood sugar control with oral medications, injectable therapies such as GLP-1 receptor agonists and insulin may be prescribed.
3. Insulin Therapy:
- Basal Insulin: Provides a steady release of insulin throughout the day to control fasting blood sugar levels.
- Bolus Insulin: Administered before meals to control postprandial (after-meal) blood sugar spikes.
- Premixed Insulin: Combines both basal and bolus insulin in a single injection for convenience.
4. Regular Monitoring and Follow-Up:
- Self-Monitoring of Blood Glucose (SMBG): Individuals with Type 2 DM should monitor their blood sugar levels regularly using a glucometer to track their response to treatment and make adjustments as needed.
- HbA1c Testing: Measures average blood sugar levels over the past two to three months and is used to assess long-term glucose control and treatment effectiveness.
- Regular Check-Ups: Routine follow-up visits with healthcare providers are essential for monitoring blood sugar levels, assessing for complications, adjusting treatment plans, and providing ongoing education and support.
Read more:

