Deep Vein Thrombosis (DVT);
- Overview
- What is Deep Vein Thrombosis (DVT)?
- Causes of DVT:
- Virchow’s Triad
- Additional Causes
- Risk Factors For Deep Vein Thrombosis:
- Signs and Symptoms of DVT:
- Diagnosis of Deep Vein Thrombosis:
- History:
- Clinical Examination:
- Radiology
- Clinical Decision Rules
- Point-of-Care Ultrasound (POCUS)
- Treatment of DVT:
- Complications Of DVT:
- Pulmonary Embolism (PE)
- Post-Thrombotic Syndrome (PTS)
- Recurrent Venous Thromboembolism (VTE)
- Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
- Venous Gangrene
- Compartment Syndrome
- Superficial Thrombophlebitis
- Stroke or Systemic Embolism
- Phlegmasia Alba Dolens (PAD) and Phlegmasia Cerulea Dolens (PCD)
- Summary:
Overview
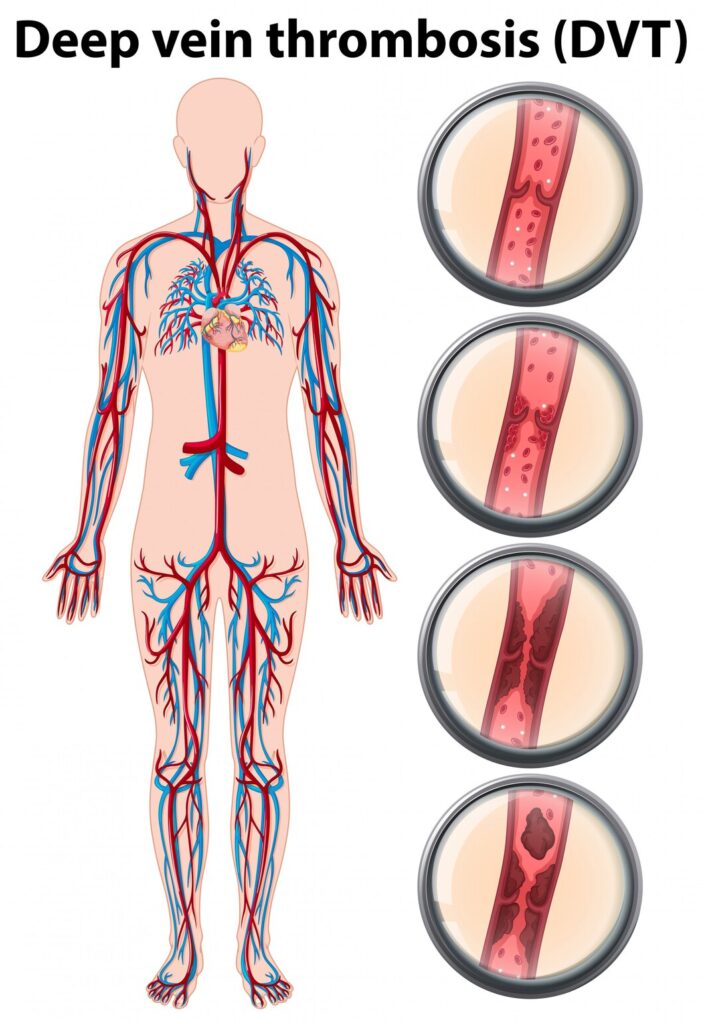
Deep Vein Thrombosis (DVT) is a serious medical condition characterized by the formation of blood clots within deep veins, typically in the legs. These clots can pose significant health risks if they break loose and travel to vital organs, causing life-threatening complications such as pulmonary embolism.
What is Deep Vein Thrombosis (DVT)?
DVT occurs when a blood clot forms in one or more of the deep veins in your body, usually in the legs. These clots can obstruct blood flow, leading to swelling, pain, and potentially severe complications. If left untreated, DVT can result in permanent damage to the affected veins and organs.
Causes of DVT:
The primary cause of DVT is sluggish blood flow, often due to prolonged periods of inactivity or immobility. Other contributing factors may include injury to the veins, surgery, certain medical conditions such as cancer or inflammatory diseases, and genetic predispositions that affect blood clotting. Let’s know them:
Virchow’s Triad
Virchow’s triad consists of three primary factors that contribute to the formation of blood clots:
- Endothelial Injury: Damage to the endothelial lining of blood vessels disrupts the normal anticoagulant properties of the blood vessel wall, promoting clot formation. Injury can result from surgery, trauma, or inflammation.
- Hypercoagulability: Conditions that increase blood clotting tendencies, such as cancer, pregnancy, genetic disorders, or certain medications, can tip the balance towards clot formation.
- Blood Stasis: Sluggish blood flow or stasis, often due to immobility, obesity, or compression of veins, allows blood to pool and clot, particularly in the lower extremities.
Additional Causes
- Venous Obstruction: External compression or internal obstruction of veins, caused by factors like tight clothing, casts, tumors, or enlarged organs, disrupts blood flow and promotes clot formation.
- Hormonal Factors: Estrogen-containing medications, hormonal contraceptives, and hormone replacement therapy can alter blood clotting dynamics, increasing the risk of DVT, particularly in women.
- Age and Genetics: Advanced age and genetic predispositions, such as Factor V Leiden mutation, influence blood vessel integrity and clotting mechanisms, contributing to DVT risk.
Risk Factors For Deep Vein Thrombosis:
Several factors increase the risk of developing DVT, including:
- Prolonged Immobility: Extended periods of sitting or bed rest can impede blood flow and increase clot formation.
- Surgery or Trauma: Recent surgery, particularly orthopedic procedures involving the lower limbs, and traumatic injuries can elevate DVT risk.
- Advanced Age: Older adults are more susceptible to DVT due to natural changes in blood vessel structure and function.
- Family History: A family history of blood clotting disorders or DVT can predispose individuals to the condition.
- Obesity: Excess weight can strain veins and hinder proper blood circulation, raising the likelihood of clot formation.
Signs and Symptoms of DVT:
Recognizing the signs and symptoms of DVT is crucial for early detection and treatment. Common indicators include:
- Swelling: Persistent swelling, usually in one leg, is a typical symptom of DVT.
- Pain: The affected area may feel tender or painful, especially when standing or walking.
- Redness and Warmth: The skin over the clot site may appear reddish and feel warm to the touch.
- Visible Veins: In some cases, the affected veins may become more visible or prominent.
Diagnosis of Deep Vein Thrombosis:
Diagnosing DVT typically involves a combination of medical history review, physical examination, and diagnostic tests such as:
- Ultrasound: This non-invasive imaging test uses sound waves to visualize blood flow and detect clots in the veins.
- D-Dimer Test: Elevated levels of D-dimer, a protein fragment produced when a blood clot dissolves, may indicate the presence of DVT.
- Venography: In this procedure, a contrast dye is injected into a vein, allowing doctors to monitor blood flow and identify clots using X-ray imaging.
Let’s see way to Diagnose DVT case in a more clinical way:
History:
Majority of patients will present to you with these symptoms:
- Pain (50% of patients)
- Redness
- Swelling (70% of patients)
Clinical Examination:
On examination, you may find:
- Limb edema may be unilateral or bilateral if the thrombus extends to pelvic veins.
- Red and hot skin with dilated veins
- Tenderness
Clinical Probability Assessment
- Assess using the Wells scoring system.
- Clinical probability is low for patients scoring 0 to 1; for those with a score of 2 or above, the probability is high.
Blood Tests:
After clinically examining the patient, if you suspect DVT then these tests will aid your clinical suspicion:
- D-dimer test (very sensitive but not very specific)
- Coagulation profile (PT-INR, BT, CT etc)
Imaging
- Proximal leg vein ultrasound
- Positive result indicates DVT.
- Repeat within 24 hours if initial test is negative.
Diagnostic Algorithm
- High Probability (Wells score ≥ 2)
- Immediate proximal leg vein ultrasound or D-dimer test.
- If imaging not possible, administer parenteral anticoagulant.
- Low Probability (Wells score < 2) with Positive D-dimer
- Immediate proximal leg vein ultrasound or parenteral anticoagulant if imaging not feasible.
Follow-up
- Repeat proximal leg vein ultrasound if D-dimer positive and initial ultrasound negative.
- Consider repeat testing or D-dimer test in one to two weeks for calf DVT.
Radiology
- Doppler ultrasonography
- MRI venography
- CT venograms
Clinical Decision Rules
- Utilize Pulmonary Embolism Rule-Out Criteria (PERC) and Wells Criteria for risk stratification.
- D-dimer test selectively used in low-probability patients without confounding diagnoses.
Point-of-Care Ultrasound (POCUS)
- Two-point compression exam: femoral and popliteal veins.
- Increase venous distention with reverse Trendelenburg.
- Complete collapse of vein rules out DVT.
- Repeat testing may be required for negative results.
Treatment of DVT:
The primary goals of DVT treatment are to prevent clot growth, alleviate symptoms, and reduce the risk of complications. Common treatment approaches include:
- Anticoagulant Medications: Blood-thinning medications such as heparin and warfarin help prevent new clots from forming and reduce the size of existing ones.
- Thrombolytics: In severe cases, thrombolytic drugs may be administered to dissolve large clots quickly.
- Compression Therapy: Wearing compression stockings can improve blood circulation and alleviate swelling and discomfort.
Complications Of DVT:
If left untreated or inadequately managed, DVT can lead to serious complications, including:
Pulmonary Embolism (PE)
- Embolization of thrombus to pulmonary arteries.
- Life-threatening respiratory compromise.
Post-Thrombotic Syndrome (PTS)
- Chronic venous insufficiency following DVT.
- Symptoms: pain, swelling, skin changes, ulcers.
Recurrent Venous Thromboembolism (VTE)
- Subsequent DVT or PE episodes.
- Increases morbidity, mortality.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
- Persistent pulmonary hypertension post-pulmonary emboli.
- Causes right heart strain, failure.
Venous Gangrene
- Tissue necrosis from extensive venous thrombosis.
- Requires urgent intervention.
Compartment Syndrome
- Increased muscle compartment pressure.
- Causes tissue ischemia, necrosis.
Superficial Thrombophlebitis
- Inflammation, clot formation in superficial veins.
- Can extend to deep veins, causing DVT.
Stroke or Systemic Embolism
- Thrombus dislodgement, embolization to cerebral or systemic circulation.
- Results in ischemic stroke or systemic complications.
Phlegmasia Alba Dolens (PAD) and Phlegmasia Cerulea Dolens (PCD)
- Rare conditions resulting from acute, extensive venous thrombosis.
- PAD: Severe swelling, pain, pale limb.
- PCD: Complete occlusion of venous outflow and arterial inflow, severe ischemia, blue limb.
- Both are medical emergencies with high morbidity and mortality.
Summary:
Deep Vein Thrombosis is a significant health concern that requires prompt diagnosis and appropriate treatment to prevent potentially life-threatening complications. Understanding the risk factors, signs, and symptoms of DVT is essential for early detection and intervention, ultimately improving patient outcomes and quality of life.
Read More:

