History
A 25-year-old woman presents with fatigue, weight loss, and night sweats over the past few months. She reports intermittent fever and muscle pain. Recently, she has noticed diminished pulses in her arms and episodes of dizziness.
General Examination
Upon general examination, the following findings are noted:
- Pulse: 82 beats per minute, weak in both radial arteries.
- Blood Pressure: 120/80 mmHg in the left arm, 90/60 mmHg in the right arm.
- Respiratory Rate: 18 breaths per minute.
- SpO2: 98% on room air.
Systemic Examination
Respiratory System (RS)
- Clear breath sounds bilaterally.
- No wheezes or crackles.
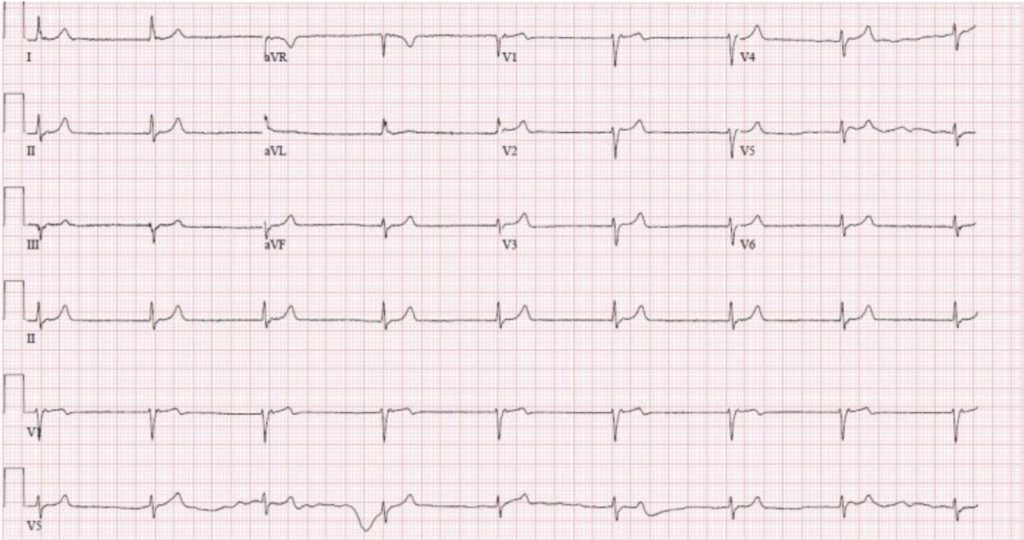
Cardiovascular System (CVS)
- Weak radial pulses bilaterally.
- Bruits heard over the subclavian and carotid arteries.
- No murmurs or gallops.
- Normal heart sounds.
Per Abdomen (PA)
- Soft and non-tender.
- No organomegaly.
- Bowel sounds present.
Central Nervous System (CNS)
- Alert and oriented.
- Normal cranial nerve function.
- No focal neurological deficits.
Laboratory Investigations
Initial laboratory tests are crucial for assessing inflammation and ruling out other conditions. Important findings include:
- Erythrocyte Sedimentation Rate (ESR): 70 mm/hr (elevated).
- C-reactive Protein (CRP): 45 mg/L (elevated).
- Complete Blood Count (CBC): Within normal limits.
- Antinuclear Antibody (ANA): Negative.
Imaging Studies
Imaging studies confirm the diagnosis. The following modalities are typically used:

- Magnetic Resonance Angiography (MRA): Reveals narrowing and thickening of the aorta and its major branches.
- Computed Tomography Angiography (CTA): Shows detailed images of the blood vessels, highlighting stenosis and occlusions.
- Ultrasound: Detects vessel wall thickening and reduced blood flow in affected arteries.
Diagnosis
The diagnosis of Takayasu arteritis is based on clinical criteria, laboratory findings, and imaging results. The American College of Rheumatology (ACR) criteria for TA include:
- Age at disease onset <40 years
- Claudication of extremities
- Decreased brachial artery pulse
- Blood pressure difference >10 mmHg between arms
- Bruit over subclavian arteries or aorta
- Arteriographic abnormalities
Meeting at least three of these criteria suggests a diagnosis of TA.
Treatment
Medical Management
The primary goal of treatment is to reduce inflammation and prevent vascular complications. Common medications include:
- Corticosteroids: High-dose prednisone is the first-line treatment to control inflammation.
- Immunosuppressants: Methotrexate or azathioprine may be used for steroid-sparing effects.
- Biologic agents: Tocilizumab, an IL-6 receptor antagonist, has shown promise in refractory cases.
Surgical Interventions
In cases of severe arterial stenosis or occlusion, surgical intervention may be necessary. Options include:
- Angioplasty: To widen narrowed arteries.
- Stenting: To keep the arteries open.
- Bypass surgery: To create a new path for blood flow around blocked arteries.
Prognosis
The prognosis for patients with Takayasu arteritis varies. With early diagnosis and appropriate treatment, many patients achieve remission and lead relatively normal lives. However, some may experience relapses or complications such as aneurysms, hypertension, or organ ischemia.
Conclusion
Takayasu arteritis, though rare, poses significant diagnostic and therapeutic challenges. A high index of suspicion, thorough clinical evaluation, and appropriate use of imaging and laboratory tests are essential for early diagnosis. Prompt and effective treatment can greatly improve outcomes, underscoring the importance of multidisciplinary care in managing this complex condition.
Read More: TAKAYASU ARTERITIS