Benign prostatic Hyperplasia (BPH);
Overview:
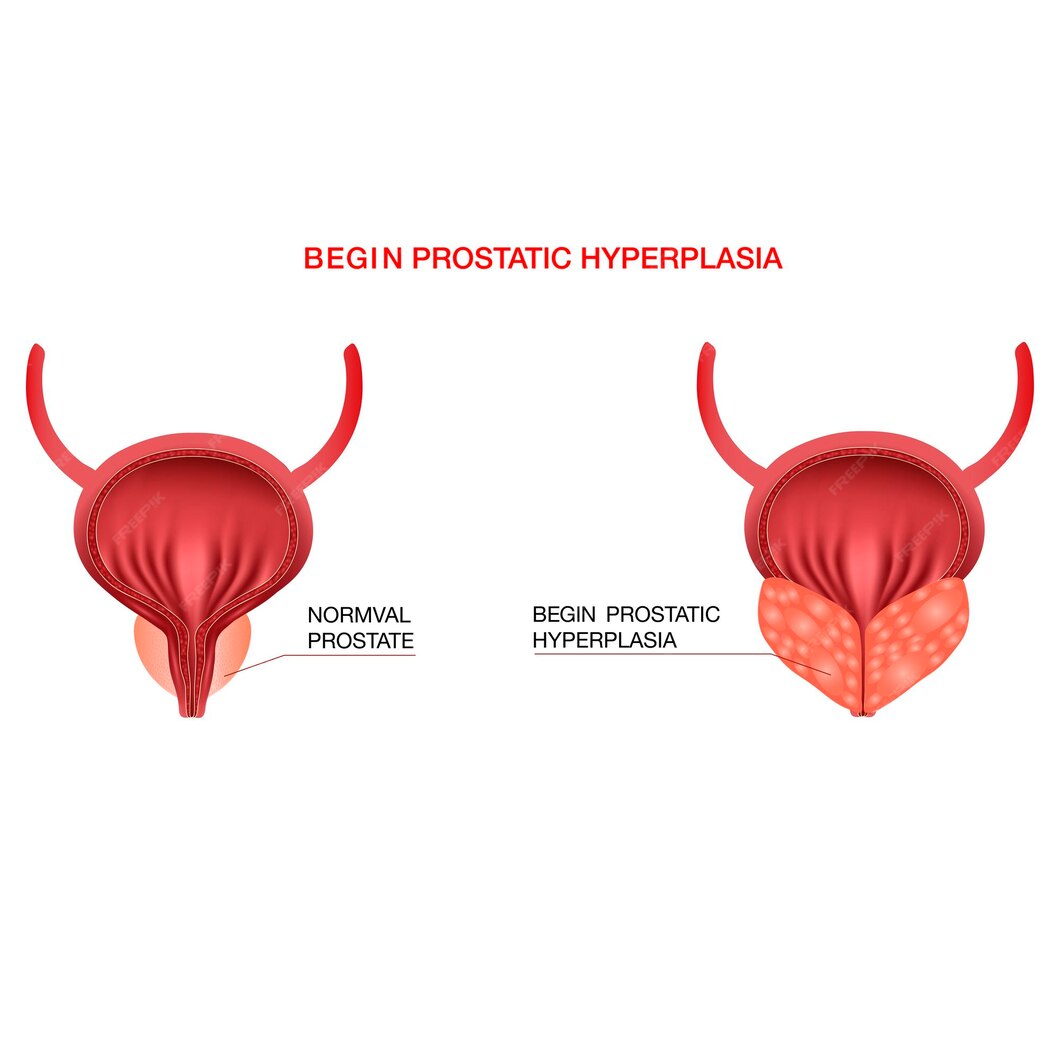
Benign prostatic hyperplasia (BPH) is a prevalent condition affecting aging men, characterized by non-cancerous growth of the prostate gland. As men age, the prostate gland, located beneath the bladder, may enlarge, leading to various urinary symptoms. Understanding the intricacies of BPH is crucial for timely diagnosis and effective management.
What is Benign Prostatic Hyperplasia (BPH)?
Benign prostatic hyperplasia refers to the enlargement of the prostate gland due to the proliferation of both glandular and stromal cells. This non-malignant growth can cause compression of the urethra, leading to urinary obstruction and bothersome lower urinary tract symptoms (LUTS).
Signs and Symptoms:
Benign prostatic hyperplasia (BPH) is a prevalent condition among aging men, characterized by the non-cancerous enlargement of the prostate gland. Common symptoms are:
1. Increased Urinary Frequency:
One of the hallmark signs of BPH is an increased need to urinate, particularly during the day. Men with BPH often find themselves making more frequent trips to the bathroom, which can disrupt daily activities and sleep patterns.
2. Urinary Urgency:
Individuals with BPH may experience a sudden and compelling urge to urinate, even when the bladder is not full. This urgency can be bothersome and may lead to anxiety or discomfort, especially when access to a restroom is limited.
3. Difficulty Initiating Urination:
BPH can cause difficulties in initiating urination, characterized by a delayed or hesitant start to the urinary stream. Men may experience straining or pushing during urination, making it challenging to empty the bladder completely.
4. Weak Urine Stream:
A weakened urine stream is another common symptom of BPH. The flow of urine may be slow, weak, or interrupted, making it difficult to empty the bladder efficiently. This can lead to a sensation of incomplete emptying after urination.
5. Intermittent Urination:
Intermittent urination refers to a start-stop pattern of urination, where the flow of urine is not continuous but rather starts and stops abruptly. This can be frustrating and may prolong the time spent in the restroom.
6. Nocturia:
Nocturia, or waking up at night to urinate, is prevalent in individuals with BPH. Men may experience multiple episodes of nocturia, disrupting their sleep and leading to daytime fatigue and decreased productivity.
7. Urinary Retention:
In severe cases of BPH, urinary retention may occur, wherein the bladder does not completely empty during urination. This can lead to discomfort, urinary tract infections, and potential complications if left untreated.
8. Incontinence:
BPH can also contribute to urinary incontinence, characterized by the involuntary leakage of urine. Men may experience dribbling or leakage of urine, particularly after urination or during physical activity.
9. Bladder Stones or Infections:
Chronic urinary retention associated with BPH may increase the risk of developing bladder stones or urinary tract infections. These complications can cause additional discomfort and require medical intervention.
10. Hematuria:
Hematuria, or blood in the urine, may occur in some cases of BPH. While not always present, hematuria should prompt further evaluation by a healthcare professional to rule out other potential causes.
Causes:
The exact cause of benign prostatic hyperplasia remains unclear. However, several factors are believed to contribute to its development, including:
- Age-related hormonal changes, particularly an increase in dihydrotestosterone (DHT).
- Hormonal imbalances, such as alterations in testosterone and estrogen levels.
- Genetic predisposition.
- Chronic inflammation of the prostate gland.
- Lifestyle factors, including obesity and sedentary behavior.
Risk Factors:
Certain factors may increase the risk of developing BPH, including:
1. Advancing Age:
Age is the primary risk factor for the development of BPH. As men age, the likelihood of experiencing prostate enlargement increases significantly. BPH is rare in men younger than 40 but becomes increasingly prevalent with each passing decade.
2. Family History:
A family history of BPH or prostate cancer may predispose an individual to developing BPH. Genetic factors play a role in the development of prostate conditions, and men with a family history of BPH are at a higher risk of experiencing prostate enlargement themselves.
3. Hormonal Imbalances:
Hormonal imbalances, particularly changes in testosterone and estrogen levels, may contribute to the development of BPH. As men age, testosterone levels may decrease while estrogen levels increase, leading to alterations in the hormonal milieu that can promote prostate growth.
4. Obesity and Unhealthy Lifestyle Habits:
Obesity and unhealthy lifestyle habits, such as poor diet and lack of exercise, have been linked to an increased risk of BPH. Excess body weight and sedentary behavior may exacerbate hormonal imbalances and inflammation, contributing to prostate enlargement.
5. Hormonal Therapy for Prostate Cancer:
Men who undergo hormonal therapy for prostate cancer may be at an increased risk of developing BPH. Hormonal treatments that reduce testosterone levels can inadvertently promote prostate growth, leading to the development of BPH symptoms.
6. Diabetes and Metabolic Syndrome:
Diabetes and metabolic syndrome, characterized by insulin resistance, obesity, and high blood pressure, have been associated with an increased risk of BPH. The underlying metabolic disturbances in these conditions may contribute to prostate enlargement.
7. Red Meat Consumption:
High consumption of red meat, particularly processed and high-fat meats, has been associated with an increased risk of BPH. The saturated fats and potential carcinogens found in red meat may contribute to inflammation and oxidative stress, which can promote prostate enlargement.
8. Erectile Dysfunction:
There is evidence to suggest that erectile dysfunction (ED) may be a risk factor for BPH. The relationship between ED and BPH is complex and multifaceted, with shared risk factors such as age, obesity, and hormonal imbalances potentially contributing to both conditions.
9. Sedentary Lifestyle:
A sedentary lifestyle, characterized by lack of physical activity and prolonged sitting, may increase the risk of developing BPH. Regular exercise has been shown to have beneficial effects on prostate health and may help reduce the risk of prostate enlargement.
10. Ethnicity:
Certain ethnicities, such as African American men, have been found to have a higher prevalence of BPH compared to other racial groups. The reasons for these disparities are not fully understood but may involve genetic, environmental, and socioeconomic factors.
Treatment:
Treatment for benign prostatic hyperplasia (BPH) aims to alleviate symptoms, improve quality of life, and prevent complications. Here’s an overview of the various treatment options available:
1. Watchful Waiting:
- In cases of mild symptoms or when symptoms are not bothersome, a watchful waiting approach may be recommended.
- Regular monitoring of symptoms and prostate health is essential to detect any progression of the condition.
2. Lifestyle Modifications:
- Making lifestyle changes such as reducing caffeine and alcohol intake, avoiding fluids before bedtime, and practicing pelvic floor exercises can help alleviate urinary symptoms.
- Maintaining a healthy weight through diet and exercise may also have a positive impact on BPH symptoms.
3. Medications:
- Alpha-Blockers: These medications relax the muscles of the prostate and bladder neck, improving urine flow and reducing symptoms such as urinary urgency and frequency.
- 5-Alpha-Reductase Inhibitors: These medications help shrink the prostate gland by blocking the conversion of testosterone to dihydrotestosterone (DHT), thereby reducing prostate size and relieving symptoms.
- Combination Therapy: Some patients may benefit from a combination of alpha-blockers and 5-alpha-reductase inhibitors for more significant symptom relief.
4. Minimally Invasive Procedures:
- Transurethral Microwave Thermotherapy (TUMT): This procedure uses microwave energy to heat and destroy prostate tissue, relieving urinary symptoms.
- Transurethral Needle Ablation (TUNA): TUNA involves the insertion of needles into the prostate gland, where radiofrequency energy is used to heat and destroy excess tissue, improving urine flow.
- Laser Therapy: Various laser therapies, such as Holmium laser enucleation of the prostate (HoLEP) and photoselective vaporization of the prostate (PVP), are used to remove or shrink prostate tissue, alleviating symptoms.
5. Surgical Intervention:
- Transurethral Resection of the Prostate (TURP): TURP is a surgical procedure in which a portion of the prostate gland is removed using a resectoscope inserted through the urethra. It is considered the gold standard treatment for BPH in men with moderate to severe symptoms.
- Open Prostatectomy: In cases of very large prostate glands, open prostatectomy may be necessary to remove the obstructing tissue.
- Prostatic Urethral Lift (UroLift): This minimally invasive procedure involves the placement of implants to lift and hold the enlarged prostate tissue away from the urethra, improving urine flow.
6. Experimental Therapies:
- Several emerging therapies, such as prostatic artery embolization (PAE) and aquablation therapy, are being investigated as alternative treatment options for BPH. These therapies aim to reduce prostate volume and improve urinary symptoms while minimizing side effects.
7. Combination Approaches:
- Depending on the severity of symptoms and individual patient factors, a combination of lifestyle modifications, medications, minimally invasive procedures, and surgical intervention may be recommended to achieve optimal symptom relief and improve quality of life.
Differential Diagnosis:
It is very essential for physicians to diagnose BPH properly keeping in mind the potential differentials. It might be from simple UTI to dangerous prostate cancer. Let’s know the DD’s;
- Urinary Tract Infections (UTIs):
UTIs exhibit symptoms similar to BPH but are accompanied by fever and cloudy urine, setting them apart. - Prostate Cancer:
Bone pain and elevated PSA levels signal potential prostate cancer, necessitating further investigation. - Overactive Bladder (OAB):
OAB presents with a sudden urge to urinate, distinguishing it from BPH. - Urinary Retention:
Neurological evaluation helps differentiate urinary retention from BPH. - Neurogenic Bladder:
Conditions like spinal cord injury may mimic BPH symptoms, warranting thorough assessment. - Urethral Stricture:
Symptoms like weak stream and hesitancy indicate urethral stricture. - Bladder Outlet Obstruction (BOO):
Urodynamic studies help identify the underlying causes of bladder outlet obstruction. - Diabetes Mellitus:
Polyuria and polydipsia differentiate diabetes from BPH, guiding diagnosis. - Medication Side Effects:
Medication history reveals potential contributors to urinary symptoms. - Pelvic Organ Prolapse:
Pelvic examination aids in diagnosing prolapse-related urinary symptoms.
This systematic approach aids in accurate diagnosis and tailored treatment plans for patients with BPH.
Lifestyle Modifications:
In addition to medical interventions, lifestyle modifications can play a significant role in managing BPH symptoms. These may include:
- Maintaining a healthy weight through diet and regular exercise.
- Limiting fluid intake, especially before bedtime, to reduce nocturia.
- Avoiding caffeine and alcohol, which can irritate the bladder.
- Practicing pelvic floor exercises to improve bladder control.
- Managing stress and anxiety, which can exacerbate urinary symptoms.
Prevention:
While benign prostatic hyperplasia may be an inevitable part of aging for many men, certain preventive measures may help reduce the risk or delay its onset. These include:
- Maintaining a healthy lifestyle, including regular exercise and a balanced diet.
- Avoiding smoking and excessive alcohol consumption.
- Seeking prompt medical attention for urinary symptoms to prevent complications.
- Regular prostate screenings, especially for individuals with a family history of BPH or prostate cancer.
In conclusion, benign prostatic hyperplasia is a common condition that can significantly impact a man’s quality of life.

