Vitiligo;
Overview:
Vitiligo is a chronic skin condition characterized by the loss of pigment, resulting in patches of depigmented skin. This condition affects individuals of all ages, genders, and ethnic backgrounds and can have a significant impact on both physical appearance and psychological well-being.
What is Vitiligo?
Vitiligo occurs when melanocytes, the cells responsible for producing melanin, are destroyed or become dysfunctional. As a result, affected areas of the skin lose their natural color and become lighter or completely white in patches.

How Does Vitiligo Begin?
Vitiligo starts subtly, often with small changes that grow over time. Anyone can develop vitilligo at any age. While the exact cause isn’t fully understood, several factors play a role:
Early Signs:
- Small, pale patches appear on the skin.
- Borders between affected and normal skin become noticeable.
- These patches can slowly grow and spread.
Possible Triggers:
- Genetic Factors: Family history increases the risk.
- Autoimmune Dysfunction: Immune system attacks pigment-producing cells.
- Environmental Triggers: Chemicals, trauma, or stress may contribute.
Progression:
- Patches may enlarge and spread unpredictably.
- Physical trauma or emotional stress can worsen symptoms.
What Causes Vitiligo?
The exact cause of vitiligo remains unclear, but it is believed to involve a combination of genetic, autoimmune, and environmental factors. Genetic predisposition, autoimmune disorders, oxidative stress, and exposure to certain chemicals or trauma are thought to contribute to the development of vitilligo.
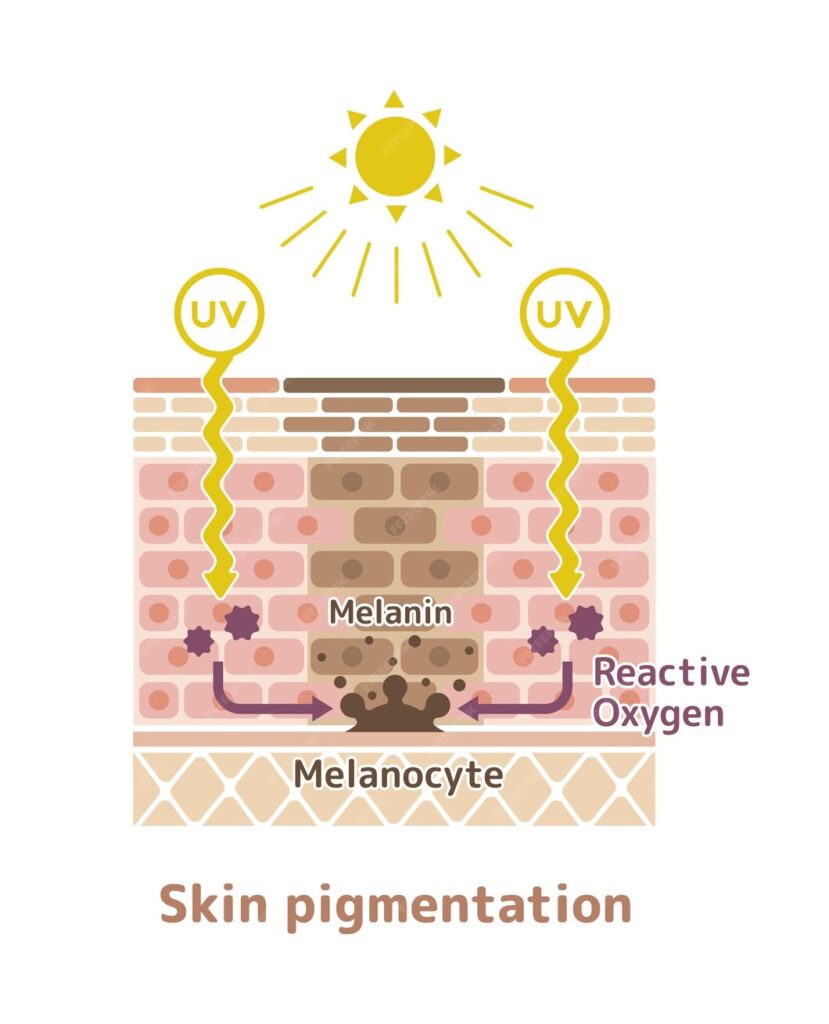
1. Absence of Melanin Pigment
Vitiligo is primarily characterized by the absence of melanin pigment in certain areas of the skin, leading to depigmented patches. The main cause of this pigment loss is the destruction or dysfunction of melanocytes, the specialized cells responsible for producing melanin.
2. Mechanism of Destruction of Melanocytes:
The mechanism underlying vitilligo involves the targeted destruction of melanocytes. Several factors contribute to this process:
- Autoimmune Attack: In many cases, vitiligo is considered an autoimmune disorder, where the body’s immune system mistakenly identifies melanocytes as foreign invaders and attacks them. This autoimmune response leads to the destruction of melanocytes and subsequent loss of pigment in the affected areas of the skin.
- Oxidative Stress: Oxidative stress, characterized by an imbalance between reactive oxygen species (ROS) production and antioxidant defenses, can also contribute to the destruction of melanocytes. ROS can induce cellular damage and trigger apoptosis (cell death) in melanocytes, further exacerbating pigment loss in vitiligo.
- Neurogenic Factors: Emerging evidence suggests that neurogenic factors may also play a role in the development of vitilligo. Neurochemical changes and alterations in neurogenic signaling pathways may influence melanocyte function and survival, contributing to the pathogenesis of the condition.
- Genetic Predisposition: While the exact genetic factors underlying vitiligo remain unclear, there is evidence to suggest that genetic predisposition plays a role in the susceptibility to the condition. Certain genetic variations may increase the risk of developing Vitilligo or influence the severity and progression of the disease.

JL Herbals Bakuchi Oil 100ml (3.5 fl.oz) | Babchi | Psoralea corylifolia
Symptoms of Vitilligo:
Vitilligo presents with distinct symptoms that are characterized by depigmentation of the skin. Common signs and symptoms include:
- Depigmented Patches: The hallmark symptom of vitiligo is the presence of depigmented patches on the skin. These patches may vary in size, shape, and location and can occur anywhere on the body.
- Irregular Borders: Depigmented patches often have irregular borders, with clear distinctions between the affected and unaffected skin.
- Progressive Spreading: In many cases, vitilligo is progressive, with depigmented patches gradually enlarging and spreading over time. The rate of progression varies from person to person.
- Symmetrical Distribution: Vitilligo patches often appear symmetrically on both sides of the body, although they may also occur in a non-symmetrical pattern.
- Involvement of Mucous Membranes: In some cases, vitiligo may also affect mucous membranes, such as the lips, mouth, and genital area, leading to depigmentation in these areas.
Types of Vitiligo:
Vitiligo can be classified into different types based on various factors, including the distribution and pattern of depigmented patches. The main types of vitilligo include:
- Generalized Vitiligo: This is the most common type of vitilligo, characterized by widespread depigmented patches that can occur on any part of the body, including the face, hands, arms, and feet.
- Segmental Vitiligo: Segmental vitilligo typically affects one side of the body and tends to occur at a younger age than generalized vitilligo. It often progresses rapidly but may stabilize after a certain period.
- Localized or Focal Vitiligo: In localized or focal vitiligo, depigmented patches are confined to specific areas of the body, such as the hands, face, or around body orifices. This type of vitiligo may remain stable or progress slowly over time.
- Acrofacial Vitiligo: Acrofacial vitiligo affects the fingers and toes, as well as the face, particularly around the eyes and mouth. It may occur in combination with other types of vitiligo or as an isolated condition.
- Universal Vitiligo: Universal vitiligo refers to the complete or near-complete depigmentation of the skin, affecting more than 80% of the body surface area. This type of vitiligo is relatively rare but can have a significant impact on the individual’s appearance and quality of life.
Risk Factors:
Several factors may increase the risk of developing vitilligo, including:
- Family history of vitiligo or autoimmune diseases
- Presence of other autoimmune disorders, such as thyroid disease or type 1 diabetes
- Exposure to certain environmental triggers, such as chemicals or stress
- Skin trauma, such as cuts, burns, or infections
Treatment:
While there is no cure for vitiligo, several treatment options are available to manage the condition and improve skin appearance:
- Topical Corticosteroids: These medications help reduce inflammation and repigment the affected areas of the skin.
- Topical Calcineurin Inhibitors: These drugs modulate the immune response and can be effective in treating vitilligo, especially in sensitive areas such as the face and genitals.
- Phototherapy: Light-based treatments, including narrowband UVB therapy and excimer laser therapy, can stimulate melanocyte activity and promote repigmentation of the skin.
- Depigmentation: In cases of extensive vitilligo, depigmentation therapy may be recommended to lighten the unaffected areas of the skin to match the depigmented patches.
- Surgical Interventions: Surgical procedures such as skin grafting, melanocyte transplantation, and micropigmentation can be considered for localized or refractory cases of vitilligo.
Complications:
Vitiligo can have significant psychosocial implications, including low self-esteem, depression, and social stigma. Additionally, individuals with vitiligo may be at increased risk of sunburn, skin cancer, and autoimmune diseases.
Precautions:
To minimize the risk of complications and manage vitilligo effectively, individuals are advised to:
- Protect their skin from sun exposure by wearing sunscreen and protective clothing
- Avoid trauma or injury to the skin
- Seek medical advice promptly for appropriate diagnosis and treatment
- Address any underlying autoimmune conditions or stressors contributing to the development of vitilligo
Summary:
In summary, vitilligo is a complex skin disorder characterized by the loss of pigment in patches of the skin. While the exact cause remains elusive, advancements in research have led to a better understanding of the condition and improved treatment options. By raising awareness, promoting early diagnosis, and providing comprehensive care, healthcare professionals can help individuals with vitilligo manage their condition effectively and improve their quality of life.
Frequently Asked Questions (FAQS) about Vitiligo
- Can vitiligo go away?
- In some cases, vitilligo may go away on its own, especially if the depigmented patches are small and limited. However, for many individuals, vitilligo is a chronic condition that requires ongoing management and treatment.
2. Is vitiligo bad for you?
- Vitilligo itself is not harmful to your physical health, but it can have significant psychosocial implications, including low self-esteem, depression, and social stigma. Seeking support from healthcare professionals and support groups can help individuals cope with the emotional impact of vitilligo.
3. Is vitiligo painful?
- Vitilligo is typically not painful, although some individuals may experience itching or discomfort in the affected areas of the skin. However, the emotional distress caused by vitilligo can be significant for some individuals.
4. Who gets vitiligo?
- Vitilligo can affect people of all ages, genders, and ethnic backgrounds. However, it is more common in individuals with a family history of vitilligo or autoimmune diseases.
5. How is vitiligo confirmed?
- Vitilligo is typically diagnosed based on a physical examination of the skin and medical history. In some cases, a Wood’s lamp examination or skin biopsy may be performed to confirm the diagnosis.
6. Can a normal person get vitiligo?
- Yes, vitilligo can affect anyone, regardless of their overall health or lifestyle. However, certain factors such as genetic predisposition, autoimmune disorders, and environmental triggers may increase the risk of developing vitilligo.
7. How to reduce melanin?
- There are various treatments available to reduce melanin production in the skin, including topical creams, laser therapy, and chemical peels. However, it is important to consult a dermatologist before attempting to reduce melanin, as some methods may have side effects.
8. How to increase melanin?
- Increasing melanin production in the skin can be challenging, but some strategies may help, such as exposure to sunlight, consuming foods rich in vitamins and antioxidants, and using topical products containing ingredients like tyrosine or copper peptides.
9. Can stress cause vitiligo?
- While stress alone does not cause vitilligo, it may exacerbate existing symptoms or trigger flare-ups in susceptible individuals. Managing stress through relaxation techniques, exercise, and therapy may help reduce the impact of stress on vitilligo.
10. Can vitiligo happen suddenly?
- Yes, vitilligo can occur suddenly, with depigmented patches appearing rapidly over a short period of time. However, for many individuals, vitilligo develops gradually, with patches enlarging and spreading over time.
11. How can vitiligo be avoided?
- Since the exact cause of vitilligo is not fully understood, it is challenging to prevent its onset. However, avoiding trauma to the skin, managing stress, and protecting the skin from excessive sun exposure may help reduce the risk of developing vitilligo.
12. At what age does vitiligo spread?
- Vitilligo can develop at any age, but it most commonly appears before the age of 30. The progression of vitilligo varies from person to person, with some individuals experiencing rapid spread of depigmented patches, while others may have stable or slow progression.
13. Should I marry a vitiligo?
- Whether or not to marry someone with vitilligo is a personal decision that depends on individual preferences and values. Vitilligo does not affect a person’s ability to love or be loved, and supportive relationships can play a crucial role in helping individuals cope with the challenges of living with vitilligo.
14. What celebrities have vitiligo?
- Several celebrities have openly spoken about their experiences with vitilligo, including model Winnie Harlow, actor Jon Hamm, and singer-songwriter Michael Jackson.
15. Can vitiligo appear on private parts?
- Yes, vitiligo can affect any part of the body, including the genital area. However, depigmented patches on the genitals may be less noticeable and may not require treatment unless they cause discomfort or distress. Consulting a dermatologist can help address any concerns about vitilligo on private parts.
Read more:

