Melasma;
Overview:
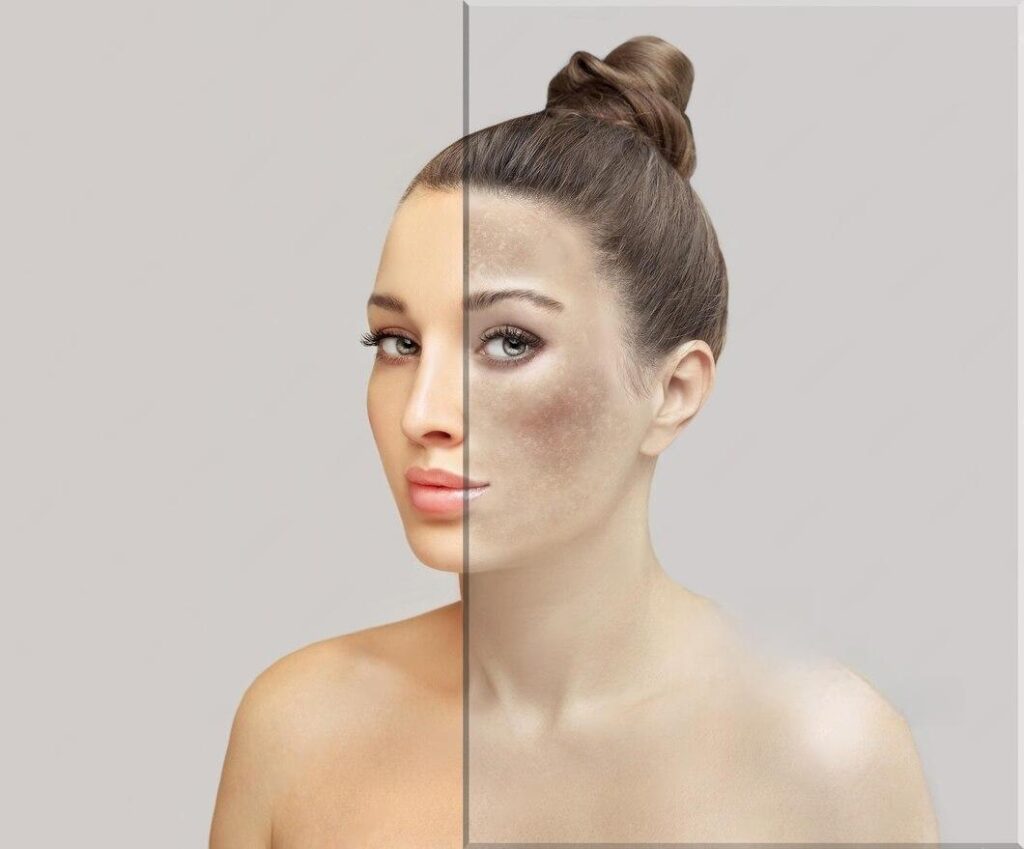
Melasma is a common skin condition characterized by the development of dark, discolored patches on the skin, primarily on the face. This condition, although not harmful, can have a significant impact on self-esteem and quality of life.
What is Melasma?
Melasma, also known as chloasma, is a chronic skin disorder characterized by the appearance of hyperpigmented patches on the face, particularly on the cheeks, forehead, chin, and upper lip. These patches typically have irregular borders and may vary in color from light brown to dark brown.
What are Causes of Melasma :
Melasma, is due to over stimulation of melanocytes in our skin. chloasma, a common skin condition characterized by hyperpigmented patches, can be influenced by various factors.
1. Genetic Influences:
- Genetic predisposition may play a significant role in the development of melasma.
- chloasma is more prevalent in females than males, and individuals with light-brown skin types from regions with high sun exposure are more susceptible.
- Approximately 50% of melasma cases report a positive family history, indicating a genetic link to the condition. Identical twins have been reported to develop chloasma, further emphasizing the genetic component.
2. Sunlight Exposure:
- Ultraviolet (UV) radiation from the sun is a major trigger for melasma.
- UV radiation can cause lipid peroxidation in cellular membranes, leading to the production of free radicals that stimulate melanocytes to produce excess melanin.
- While sunscreens that block UV-B radiation are commonly used, they may not fully protect against UV-A and visible radiation, which also stimulate melanocyte activity.
3. Hormonal Influences:
- Hormonal fluctuations, particularly during pregnancy, play a significant role in the development of chloasma.
- The “mask of pregnancy” refers to melasma that occurs in pregnant individuals, attributed to increased levels of estrogen, progesterone, and melanocyte-stimulating hormone during the third trimester.
- Melasma may also occur in individuals using hormonal contraceptives containing estrogen and progesterone or undergoing hormone replacement therapy.
- Postmenopausal women given progesterone may be more prone to chloasma development compared to those given estrogen alone, implicating progesterone in the pathogenesis of the condition.
4. Thyroid Disease:
- There is a notable association between melasma and thyroid disease.
- chloasma patients often exhibit a four-fold increase in thyroid disease prevalence.
- Additionally, there is a correlation between melasma development and the presence of melanocytic and lentiginous nevi, suggesting a relationship between pigmentation and the onset of chloasma.
Signs and Symptoms:
The primary signs and symptoms of melasma include:
1. Hyperpigmented Patches:
- The hallmark sign of melasma is the presence of hyperpigmented patches on the skin.
- These patches typically appear as dark, irregularly shaped areas of discoloration.
- Commonly affected areas include the cheeks, forehead, chin, upper lip, and bridge of the nose.
2. Symmetrical Distribution:
- Melasma patches often occur symmetrically on both sides of the face.
- This symmetrical distribution distinguishes melasma from other forms of hyperpigmentation.
3. Variation in Color and Intensity:
- Melasma patches may vary in color and intensity, ranging from light brown to dark brown.
- The color and intensity of the patches may change over time, depending on factors such as sun exposure and hormonal fluctuations.
4. Exacerbation with Sun Exposure:
- Sun exposure is a significant trigger for melasma and can exacerbate existing patches.
- Melasma patches tend to darken and become more prominent when exposed to ultraviolet (UV) radiation from the sun.
5. Commonly Affected Areas:
- While chloasma can occur on any part of the body exposed to sunlight, it most commonly affects the face.
- In addition to the typical facial distribution, chloasma may also occur on the neck and forearms in some individuals.
6. Association with Hormonal Changes:
- Melasma is often associated with hormonal changes, particularly in women.
- Pregnancy-related melasma, also known as the “mask of pregnancy,” commonly occurs during the third trimester due to hormonal fluctuations.
7. Psychological Impact:
- Beyond the physical manifestations, chloasma can have a significant psychological impact on affected individuals.
- Low self-esteem, embarrassment, and distress about changes in appearance are common emotional responses to chloasma.
Risk Factors:
Several factors may increase the risk of developing chloasma, including:
- Female Gender: chloasma is more common in women than men, especially during pregnancy or while taking hormonal contraceptives.
- Skin Type: Individuals with darker skin tones, particularly those of Hispanic, Asian, or Middle Eastern descent, are more susceptible to chloasma.
- Hormonal Factors: Hormonal fluctuations during pregnancy, hormonal therapy, or certain medical conditions may trigger or exacerbate chloasma.
Treatment:
Remember, there is no one best treatment for chloasma. Often, the most effective treatment combines sun protection with medications that you apply to your skin — and sometimes a procedure.
1. Topical Therapies:
- First-line treatment for melasma often involves topical medications, primarily in the form of triple combinations containing hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01%.
- These combinations work by inhibiting melanin production and reducing inflammation in the skin.
- If triple combinations are unavailable or contraindicated, dual ingredients or single agents may be considered.
- Avoidance of sun exposure and estrogen exposure is crucial during treatment to prevent exacerbation of chloasma.
2. Chemical Peels:
- Chemical peels can be effective in treating chloasma but carry a risk of adverse effects such as epidermal necrosis, postinflammatory hyperpigmentation, and hypertrophic scars.
- They are considered second-line therapies and should be used only if topical medications have failed.
- Peels typically use glycolic or salicylic acid-based compounds to increase turnover of hyperpigmented keratinocytes.
- Treatment often begins with monthly sessions using low concentration formulas and may progress to weekly applications at higher concentrations.
- Close monitoring of skin depigmentation is necessary during peel treatments, and therapy should be halted if adverse effects or alterations in pigmentation occur.
3. Laser Therapy:
- Laser therapy may be considered for chloasma treatment, particularly in cases of extensive disease that is refractory to other treatments.
- However, the efficacy of lasers for chloasma treatment is variable, and undesired cosmetic results may occur.
- Lasers should be used cautiously, as they may actually worsen the condition in some cases.
- Close monitoring and experienced hands are essential when considering laser therapy for chloasma.
4. Combination Therapy:
- Combining different treatment modalities, such as topical therapies, chemical peels, and laser treatments, may yield better results in some cases.
- Combination therapy should be tailored to the individual patient’s needs and treatment response.
5. Maintenance and Follow-up:
- Maintenance therapy and regular follow-up appointments are crucial for managing chloasma effectively.
- Patients should continue to use sun protection measures and avoid triggers that can exacerbate chloasma.
Complications:
While chloasma itself is not harmful, it can have significant psychosocial implications, including low self-esteem, depression, and anxiety. Additionally, chloasma patches may darken and become more resistant to treatment with continued sun exposure or hormonal fluctuations.
How to Prevent Melasma :
Preventing chloasma involves minimizing exposure to known triggers and practicing sun protection:
- Sun Protection: Use broad-spectrum sunscreen with SPF 30 or higher daily, wear protective clothing, and seek shade when outdoors.
- Hormonal Management: For women prone to chloasma, talk to your healthcare provider about hormone therapy options that may minimize the risk of chloasma flare-ups.
Understanding the causes, symptoms, and treatment options for chloasma is essential for effectively managing this common skin condition.
Frequently Asked Questions (FAQs) on Melasma
- What are the main causes of melasma?
- Melasma is primarily caused by hormonal changes, sun exposure, genetic predisposition, and certain medications or cosmetics.
2. How can I remove melasma?
- Melasma can be challenging to remove completely, but various treatments, including topical medications, chemical peels, and laser therapy, may help lighten and improve the appearance of chloasma patches.
3. What is the treatment for melasma?
- Treatment for chloasma typically involves a combination of topical therapies, such as hydroquinone cream, along with sun protection measures and lifestyle modifications.
4. How to remove melasma naturally?
- While natural remedies may offer some benefits, such as using sunscreen, wearing protective clothing, and avoiding sun exposure, they may not completely remove chloasma on their own.
5. How can I stop melasma permanently?
- Achieving permanent resolution of melasma can be challenging, but consistent sun protection, avoiding hormonal triggers, and following a personalized treatment plan recommended by a dermatologist may help manage the condition effectively.
6. Is vitamin C good for melasma?
- Vitamin C may have skin-brightening properties and can be beneficial in conjunction with other treatments for chloasma. However, its effectiveness as a standalone treatment for chloasma is limited.
7. What is the 3 cream for melasma?
- The “triple combination cream” often prescribed for chloasma contains hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01%.
8. Can tomatoes remove melasma?
- While tomatoes contain antioxidants that may benefit the skin, there is limited scientific evidence to support their effectiveness in removing chloasma.
9. Which oil is best for melasma?
- Certain oils, such as kojic acid, azelaic acid, and niacinamide, may help lighten chloasma patches. However, individual responses to these oils may vary, and it’s essential to consult with a dermatologist before use.
10. Which vitamin is best for melasma?
- Vitamins such as vitamin C and niacinamide may help improve skin tone and reduce pigmentation in chloasma. However, their effectiveness may vary depending on individual skin types and conditions.
11. Is potato good for melasma?
- Some people believe that applying potato slices or juice to the skin may help lighten chloasma patches, but scientific evidence supporting this claim is limited.
12. What is the fastest way to cure melasma?
- There is no guaranteed fast cure for chloasma, but a combination of topical treatments, sun protection, and lifestyle modifications may help improve the appearance of chloasma over time.
13. Does B12 reduce melasma?
- While vitamin B12 is essential for overall skin health, there is no evidence to suggest that it specifically reduces chloasma.
14. Can vitamin D deficiency cause melasma?
- Vitamin D deficiency is not directly linked to melasma. However, maintaining adequate levels of vitamin D is essential for overall skin health.
15. Can aloe vera remove melasma?
- Aloe vera may have soothing properties and can be beneficial for the skin, but its effectiveness in removing chloasma is limited.
16. Can kojic acid remove melasma?
- Kojic acid is a common ingredient in skin-lightening products and may help lighten chloasma patches over time. However, it should be used under the guidance of a dermatologist to avoid adverse effects.
17. Which sunscreen is best for melasma?
- Sunscreens with broad-spectrum protection and SPF 30 or higher are recommended for individuals with chloasma. Look for sunscreens that contain physical blockers like zinc oxide or titanium dioxide.
18. Can lemon juice remove melasma?
- Lemon juice contains citric acid, which may have skin-brightening properties. However, applying lemon juice directly to the skin can be harsh and may cause irritation or inflammation.
19. Which foods increase melasma?
- Certain foods and beverages, such as spicy foods, caffeine, and alcohol, may exacerbate chloasma in some individuals. It’s essential to pay attention to your diet and lifestyle factors that may trigger or worsen chloasma.
20. How to remove melanin from skin?
- Removing melanin from the skin completely is not possible or desirable. However, various treatments, including topical medications, chemical peels, and laser therapy, may help reduce excess melanin production and improve skin tone in conditions like chloasma.
• Read more:

