AstraZeneca Thrombotic Thrombocytopenia;
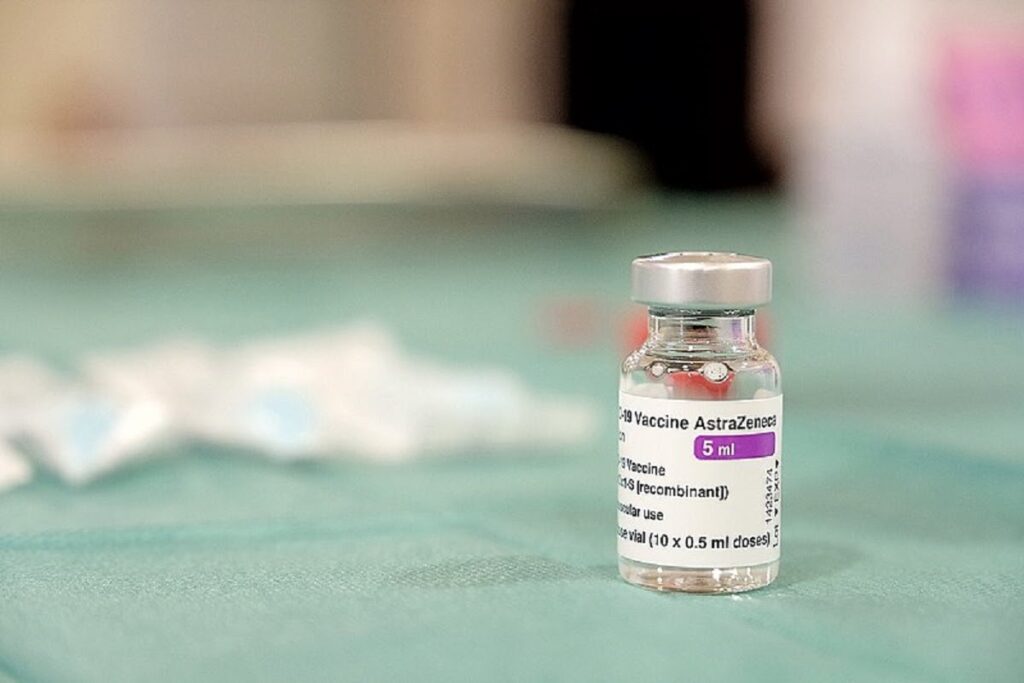
AstraZeneca Thrombotic Thrombocytopenia : Covishield side effect
In the realm of vaccination against COVID-19, recent discussions have centered around the emergence of rare side effects associated with certain vaccines. Among these, Thrombotic Thrombocytopenia Syndrome (TTS) has garnered significant attention, prompting thorough investigations and public scrutiny. In this comprehensive exploration, we delve into the intricacies of TTS, its implications, and the broader context surrounding vaccine safety.
What is Thrombotic Thrombocytopenia?
Thrombotic Thrombocytopenia Syndrome (TTS) is a rare but serious condition characterized by the simultaneous occurrence of blood clots (thrombosis) and low platelet levels (thrombocytopenia). This juxtaposition of hypercoagulability and thrombocytopenia presents a unique medical challenge, often necessitating prompt intervention and specialized care.
How it leads to blood clots in body?
The exact pathophysiological mechanisms underlying TTS remain elusive, contributing to ongoing scientific inquiries and conjectures. While the causal link between certain vaccines, notably those developed by AstraZeneca, and TTS has been acknowledged, the precise molecular pathways precipitating this phenomenon warrant further elucidation. Current hypotheses implicate immune-mediated responses triggering aberrant platelet activation and subsequent clot formation, albeit with nuances yet to be fully elucidated.
AstraZeneca’s Covishield: A Closer Look
AstraZeneca’s COVID-19 vaccine, marketed under various names including Covishield and Vaxzevria, has been at the epicenter of TTS-related discussions. The vaccine’s association with rare but potentially severe side effects has prompted regulatory scrutiny, legal actions, and public apprehensions. AstraZeneca’s acknowledgment of the vaccine’s potential to trigger TTS underscores the gravity of the situation, necessitating concerted efforts to mitigate risks while maximizing immunization benefits.
Epidemiology and Risk Factors:
Epidemiological data pertaining to TTS offer insights into its prevalence, distribution, and associated risk factors. While TTS remains a rare occurrence, discernible patterns may emerge concerning demographic predispositions, temporal associations with vaccine administration, and underlying comorbidities. Robust surveillance systems are essential for capturing and analyzing such data, enabling informed decision-making and risk stratification.
Clinical Manifestations: Symptoms
Thrombotic Thrombocytopenia Syndrome (TTS) presents a multifaceted clinical picture, encompassing thrombotic events, platelet depletion, and systemic manifestations. This comprehensive guide delves into the diverse array of signs and symptoms associated with TTS, including neurological, cardiovascular, and constitutional manifestations, while also addressing potential complications such as stroke and myocardial infarction.
1. Thrombotic Events: Clues to Hypercoagulability
- Deep Vein Thrombosis (DVT): Symptoms may include localized pain, swelling, warmth, and discoloration of the affected limb.
- Pulmonary Embolism (PE): Acute chest pain, dyspnea, hemoptysis, and hemodynamic instability may signify pulmonary embolism.
- Cerebral Venous Sinus Thrombosis (CVST): Severe headaches, focal neurological deficits, altered consciousness, and seizures may herald cerebral venous sinus thrombosis.
2. Thrombocytopenia: Insights into Platelet Depletion
- Petechiae and Ecchymoses: Small hemorrhages (petechiae) and bruise-like discolorations (ecchymoses) may occur due to impaired platelet function.
- Mucosal Bleeding: Epistaxis, gingival bleeding, and gastrointestinal hemorrhage may ensue due to diminished platelet counts.
- Hemorrhagic Bullae: Rarely, the formation of hemorrhagic bullae on the skin and mucous membranes may signify severe thrombocytopenia.
3. Constitutional Symptoms:
- Fever: Low-grade fevers may accompany the systemic inflammatory response triggered by TTS.
- Malaise and Fatigue: Generalized weakness, lethargy, and malaise may ensue, reflecting the physiological toll of TTS.
4. Neurological Manifestations:
- Severe Headache: Intense, debilitating headaches refractory to conventional analgesics may herald cerebral venous sinus thrombosis.
- Altered Mental Status: Confusion, disorientation, and cognitive deficits may manifest secondary to cerebral hypoperfusion or intracranial hemorrhage.
5. Cardiovascular Complications:
- Stroke (Cerebrovascular Accident, CVA): Sudden onset of focal neurological deficits, including hemiparesis, aphasia, and visual disturbances, may signify stroke.
- Myocardial Infarction (MI): Chest pain or discomfort, dyspnea, diaphoresis, and nausea may indicate myocardial infarction, necessitating urgent medical attention.
Complications of TTS:
- Disseminated Intravascular Coagulation (DIC): Widespread microvascular thrombosis and consumption of clotting factors and platelets may culminate in DIC.
- Organ Dysfunction: Thrombotic occlusion of vital organs such as the lungs, brain, heart, and kidneys may precipitate multi-organ dysfunction syndrome (MODS).
- Hemorrhagic Complications: Thrombocytopenia may predispose individuals to hemorrhagic complications, including intracranial hemorrhage and gastrointestinal bleeding.
Diagnostic Challenges:
Diagnostic dilemmas often accompany the evaluation of suspected TTS cases, owing to the overlap of symptoms with other medical conditions and the need for specialized investigations. Differential diagnoses encompass a broad array of thrombotic and thrombocytopenic disorders, necessitating comprehensive assessments encompassing laboratory tests, imaging modalities, and clinical evaluations.
Treatment Of Thrombotic Thrombocytopenia:
Optimal management of TTS mandates a multidisciplinary approach integrating pharmacotherapy, supportive care, and targeted interventions aimed at mitigating thrombotic complications while addressing underlying pathogenic mechanisms. Anticoagulation remains a cornerstone of therapy, albeit with nuanced considerations regarding dosage, duration, and concomitant therapies. Individualized treatment algorithms guided by clinical severity and patient-specific factors are pivotal for optimizing outcomes in TTS cases.
Regulatory Responses: Safeguarding Public Health
Regulatory agencies play a pivotal role in monitoring vaccine safety, adjudicating adverse event reports, and disseminating evidence-based recommendations to healthcare stakeholders and the general public. Timely regulatory responses, grounded in robust pharmacovigilance frameworks and scientific scrutiny, are essential for maintaining public trust, ensuring vaccine confidence, and safeguarding global health security.
Navigating the Way Forward
In navigating the complexities surrounding Thrombotic Thrombocytopenia Syndrome, a multifaceted approach encompassing scientific inquiry, clinical vigilance, regulatory oversight, and public engagement is indispensable. While challenges persist, collaborative endeavors aimed at elucidating TTS pathogenesis, refining diagnostic strategies, and optimizing treatment paradigms hold promise in mitigating risks and enhancing patient outcomes. As we traverse this uncharted terrain, vigilance, transparency, and evidence-based decision-making remain paramount in safeguarding public health amidst the ongoing battle against COVID-19.
AstraZeneca Thrombotic Thrombocytopenia

