Hyperthyroidism, a prevalent thyroid disorder, occurs when the thyroid gland becomes overactive, producing an excess of thyroid hormones. These hormones, primarily thyroxine (T4) and triiodothyronine (T3), play a pivotal role in regulating metabolism, energy levels, and bodily functions. In this comprehensive article, we will delve into the causes, types, symptoms, complications, and management of hyperthyroidism.
Causes of Hyperthyroidism
Hyperthyroidism can arise from various causes, each affecting the thyroid gland’s hormone production differently:
- Graves’ Disease: The most common cause of hyperthyroidism is Graves’ disease, an autoimmune disorder in which the immune system mistakenly produces antibodies that stimulate the thyroid gland excessively.
- Toxic Nodular Goiter: In this type, one or more nodules (abnormal growths) on the thyroid gland become overactive, leading to excessive hormone production.
- Subacute Thyroiditis: Viral infections or inflammation of the thyroid gland can cause a sudden release of stored thyroid hormones, resulting in temporary hyperthyroidism.
- Thyroiditis: Inflammation of the thyroid gland due to infection or autoimmune reactions can disrupt hormone regulation.
- Excessive Iodine: Consuming high doses of iodine, often from medications or supplements, can trigger hyperthyroidism.
- Toxic Adenomas: These are noncancerous tumors that develop on the thyroid gland, producing an excess of hormones.
- Pituitary Malfunction: Rarely, a pituitary gland tumor can stimulate excessive thyroid hormone production by releasing excessive thyroid-stimulating hormone (TSH).
Types of Hyperthyroidism
Here’s a table summarizing typical TSH (Thyroid-Stimulating Hormone), T3 (Triiodothyronine), and T4 (Thyroxine) values in primary, secondary, and tertiary hyperthyroidism:
| Hormone Levels | Primary Hyperthyroidism | Secondary Hyperthyroidism | Tertiary Hyperthyroidism |
|---|---|---|---|
| TSH Levels | Low | Low | Low |
| T3 Levels | High | High | High |
| T4 Levels | High | High | High |
| Possible Causes | Graves’ Disease, Toxic Nodular Goiter, Toxic Adenomas | Pituitary Tumor, Excess TSH | Hypothalamic Dysfunction |
| Key Characteristics | Overactive thyroid gland, low TSH due to negative feedback loop | Overactive thyroid gland, elevated TSH from pituitary | Overactive thyroid gland, low TSH, and abnormal hypothalamic regulation |
Hyperthyroidism can manifest in different forms, each with distinct characteristics:
- Primary Hyperthyroidism: This is the most common type, often caused by Graves’ disease, toxic nodular goiter, or toxic adenomas.
- Secondary Hyperthyroidism: Occurs when the pituitary gland produces excess TSH, leading to an overactive thyroid.
- Tertiary Hyperthyroidism: A rare form stemming from issues in the hypothalamus, which controls the pituitary gland’s release of TSH.
Symptoms
Hyperthyroidism can trigger a wide array of symptoms due to the accelerated metabolism caused by excess thyroid hormones:
- Weight Loss: Unexplained weight loss despite increased appetite.
- Increased Heart Rate: Rapid heartbeat (tachycardia) and palpitations.
- Nervousness: Excessive anxiety, restlessness, or irritability.
- Heat Intolerance: Feeling excessively hot and sweating profusely.
- Fatigue: Paradoxically, some individuals may experience fatigue despite hyperactivity.
- Muscle Weakness: Weak, trembling muscles and potential loss of muscle mass.
- Tremors: Hand tremors or shakiness.
- Sleep Disturbances: Difficulty falling asleep or staying asleep.
- Enlarged Thyroid (Goiter): Visible swelling in the neck.
- Eye Problems (Graves’ Disease): Eye bulging, double vision, or eye discomfort.
Ocular Manifestations of Hyperthyroidism
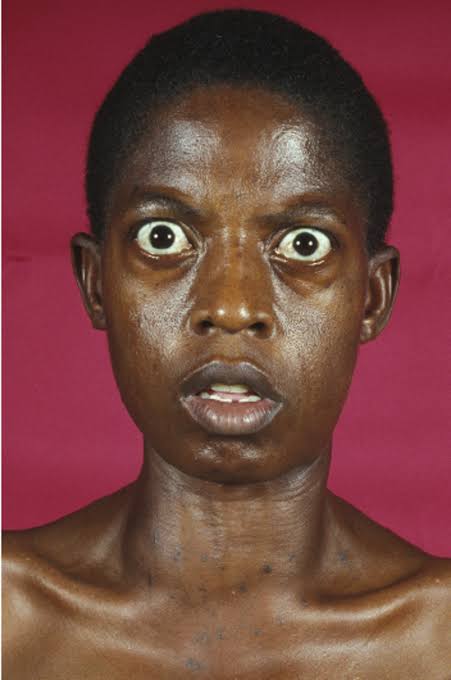
Hyperthyroidism, marked by excessive thyroid hormone production, often presents with a spectrum of distinctive ocular signs and symptoms collectively known as Graves’ ophthalmopathy (GO). Beyond proptosis and lid retraction, several other eye signs, including Stellwag’s sign, can aid in the diagnosis and management of this condition.
1. Proptosis (Exophthalmos):
Proptosis, or exophthalmos, is a hallmark feature of GO, characterized by the forward displacement of the eyeballs. This protrusion results from increased orbital fat volume and/or enlargement of the extraocular muscles, leading to a bulging appearance of the eyes.
2. Lid Retraction and Lid Lag:
Lid retraction, often accompanied by lid lag, manifests as widened palpebral apertures and a startled or wide-eyed appearance. These features are indicative of levator palpebrae superioris muscle dysfunction, contributing to the characteristic stare seen in GO patients.
3. Gaze Abnormalities:
GO can lead to various gaze-related symptoms, such as diplopia (double vision), strabismus (ocular misalignment), and restricted extraocular movements. These symptoms arise from the enlargement of the extraocular muscles, particularly the inferior and medial rectus muscles, causing mechanical restriction and altered ocular alignment.
4. Van Gogh’s Sign:
Van Gogh’s sign, named after the artist Vincent van Gogh, refers to the characteristic appearance of the eyes in GO. It presents as a widened palpebral fissure and a retracted upper eyelid, reminiscent of the almond-shaped eyes depicted in Van Gogh’s self-portraits.
5. Stellwag’s Sign:
Stellwag’s sign is observed as infrequent or incomplete blinking, often associated with ocular surface dryness and irritation. This sign reflects altered neuromuscular control of the orbicularis oculi muscle and is commonly seen in individuals with hyperthyroidism and GO.
6. Corneal Exposure and Ulceration:
Severe proptosis and lid retraction in GO can compromise eyelid closure, leading to exposure keratopathy and corneal ulceration. These complications range from mild dryness and irritation to sight-threatening ulceration, necessitating meticulous ocular surface management.
7. Optic Neuropathy:
In rare cases, GO can result in compressive optic neuropathy, characterized by optic nerve compression and ischemic injury due to orbital tissue expansion. Optic neuropathy presents with progressive visual loss, color vision deficits, and visual field defects, necessitating urgent intervention to preserve vision.
Diagnosis Of Hyperthyroidism
1. Thyroid Function Tests(TFT):
- TSH (Thyroid-Stimulating Hormone):
- Normal Range: Typically between 0.4 to 4.0 milli-international units per liter (mIU/L).
- Diagnostic Value: In primary hyperthyroidism, TSH levels are usually low, often below the reference range due to negative feedback from elevated T3 and T4 levels.
- T3 (Triiodothyronine) and T4 (Thyroxine):
- Normal Ranges: T3 levels are around 100 to 200 nanograms per deciliter (ng/dL), while T4 levels are approximately 4.5 to 11.2 micrograms per deciliter (µg/dL).
- Diagnostic Value: In hyperthyroidism, T3 and T4 levels are often elevated above the reference range.
2. Radioactive Iodine Uptake (RAIU) Test:
- This test measures how much radioactive iodine the thyroid gland absorbs. In hyperthyroidism, the thyroid gland typically has an increased uptake of radioactive iodine.
- Thyroid Scintigraphy:
- Using a radioactive tracer, this test can identify the pattern of iodine uptake by the thyroid gland. Different patterns may indicate different causes of hyperthyroidism, such as Graves’ disease or toxic nodular goiter.
3. Thyroid Ultrasound (USG):
- An ultrasound scan of the thyroid can reveal the size and structure of the gland. It can help identify nodules, inflammation, or other abnormalities.
4. Thyroid Antibody Tests:
- If autoimmune causes like Graves’ disease are suspected, specific antibody tests such as TPO (Thyroid Peroxidase) antibodies and TSI (Thyroid-Stimulating Immunoglobulin) can be conducted.
5. Fine Needle Aspiration (FNA) Biopsy:
- When thyroid nodules are present, an FNA biopsy may be performed to determine if the nodule is benign or malignant.
6. Histology (Biopsy):
- In some cases, a biopsy of thyroid tissue is necessary to examine it under a microscope and confirm specific thyroid disorders.
7. Imaging (Radiology):
- Radiological imaging such as CT scans or MRI may be used to evaluate the thyroid and surrounding structures, particularly in cases with suspected thyroid enlargement or complications.
Complications
Untreated hyperthyroidism can lead to several complications:
- Heart Issues: High blood pressure, irregular heartbeat (arrhythmia), and an increased risk of heart disease.
- Osteoporosis: Excessive thyroid hormones can weaken bones, leading to osteoporosis.
- Eye Complications (Graves’ Disease): Severe eye issues, such as vision loss, if left untreated.
- Thyroid Storm: A life-threatening condition characterized by an extreme surge in thyroid hormones, leading to high fever, rapid heart rate, and confusion.
Management
Effectively managing hyperthyroidism involves multiple strategies tailored to the underlying cause and individual patient needs:
- Medications: Antithyroid drugs, such as Methimazole and Propylthiouracil, can reduce hormone production.
- Radioactive Iodine Therapy: A targeted treatment that damages thyroid cells, reducing hormone production.
- Beta-Blockers: These drugs can alleviate symptoms like rapid heartbeat and tremors.
- Thyroidectomy: Surgical removal of all or part of the thyroid gland may be necessary in severe cases or when other treatments fail.
- Lifestyle Modifications: Adopting a balanced diet and managing stress can complement medical treatment.
- Regular Monitoring: Patients require ongoing monitoring to adjust treatment as needed and assess for potential complications.
In conclusion, hyperthyroidism is a complex thyroid disorder with various causes, types, and symptoms. Early diagnosis and appropriate management are essential to prevent complications and improve the patient’s quality of life.


Very informative
Pingback: Home - Common health conditions - ECG Oxford