Celiac disease;
Overview
Celiac disease, also known as celiac sprue or gluten-sensitive enteropathy, is a chronic autoimmune disorder affecting the small intestine. Individuals with celiac disease experience an adverse reaction to gluten, a protein found in wheat, barley, and rye. This article provides an in-depth exploration of this condition, including its causes, symptoms, diagnosis, and treatment options.
What is Celiac Disease?
Immune System Response
Celiac disease occurs when the body’s immune system mistakenly targets the lining of the small intestine in response to gluten consumption. This immune reaction damages the villi, tiny finger-like projections responsible for absorbing nutrients from food.
Genetic Predisposition
Genetic factors play a significant role in the development of celiac disease. People with specific genetic markers, such as the HLA-DQ2 and HLA-DQ8 genes, are at higher risk of developing the condition.
Causes:
Celiac disease is a complex condition influenced by both genetic and environmental factors. Understanding its causes is essential for diagnosis and management.
1. Genetic Factors
Genetic predisposition plays a significant role in the development of celiac disease. Certain genetic markers increase susceptibility, including:
- HLA-DQ2 and HLA-DQ8 Genes: The majority of individuals with celiac disease carry one or both of these genetic markers. However, not everyone with these genes develops the condition, indicating that additional factors are involved.
- Family History: Having a first-degree relative (parent, sibling, or child) with celiac disease increases the risk of developing the condition. This suggests a strong genetic component to the disease.
2. Environmental Triggers
While genetic predisposition is necessary for celiac disease to develop, environmental factors also play a crucial role. These triggers can include:
- Gluten Exposure: Gluten, a protein found in wheat, barley, and rye, is the primary environmental trigger for celiac disease. Exposure to gluten, particularly during infancy or early childhood, is believed to initiate the immune response that leads to the development of the condition.
- Early Introduction of Gluten: Studies suggest that introducing gluten-containing foods too early in an infant’s diet, especially before four months of age, may increase the risk of developing celiac disease in genetically susceptible individuals.
- Other Environmental Factors: Factors such as infections, gastrointestinal conditions, and stress may also contribute to the development of celiac disease. These factors can potentially disrupt the intestinal barrier and trigger immune responses.
3. Gut Microbiota
Emerging research suggests that alterations in the gut microbiota composition may play a role in the development of celiac disease. The gut microbiota, which consists of trillions of microorganisms living in the gastrointestinal tract, interacts with the immune system and influences its function. Imbalances in gut microbiota composition may contribute to the dysregulated immune response seen in celiac disease.
4. Epigenetic Factors
Epigenetic modifications, which alter gene expression without changing the underlying DNA sequence, may also contribute to the development of celiac disease. Environmental factors, such as diet and exposure to toxins, can influence epigenetic changes that affect the risk of developing the condition. Understanding these epigenetic mechanisms may provide insights into the complex interplay between genetics and the environment in celiac disease development.
5. Other Risk Factors
In addition to genetic and environmental factors, certain risk factors may increase the likelihood of developing celiac disease, including:
- Autoimmune Conditions: Individuals with other autoimmune conditions, such as type 1 diabetes, autoimmune thyroid disease, and autoimmune liver disease, have a higher risk of developing celiac disease.
- Gender: Celiac disease is more common in females than males, although the reasons for this gender difference are not fully understood.
Signs And Symptoms of Celiac Disease:
Celiac disease can manifest with a wide range of signs and symptoms, varying in severity and presentation. Recognizing these symptoms is crucial for timely diagnosis and management of the condition.
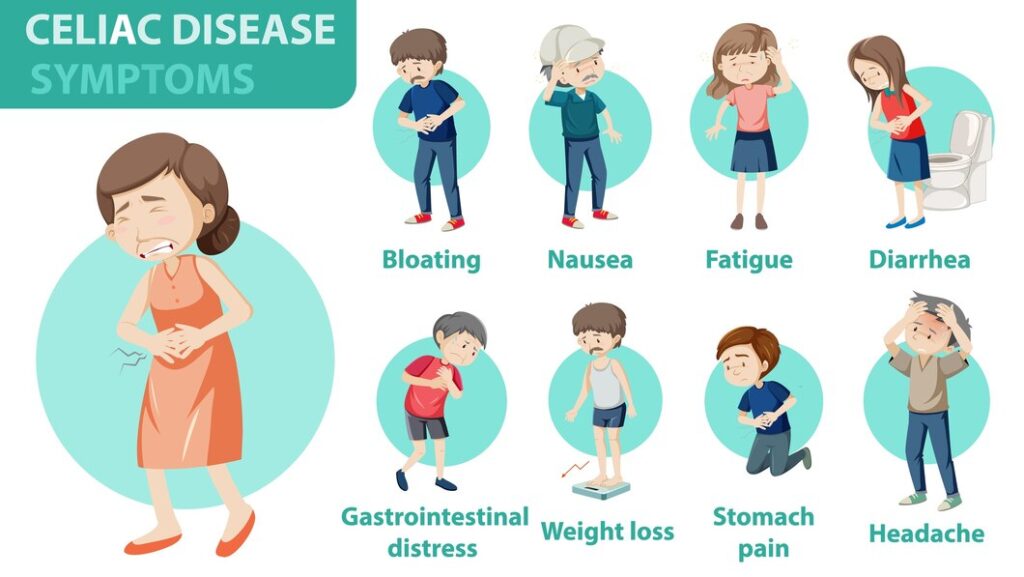
1. Gastrointestinal Symptoms
Gastrointestinal symptoms are common in celiac disease and may include:
- Chronic Diarrhea: Frequent and watery bowel movements that persist over time.
- Abdominal Pain: Discomfort or cramping in the abdominal region, often accompanied by bloating.
- Bloating: Feeling of fullness or swelling in the abdomen, often accompanied by gas.
- Constipation: Difficulty passing stools or infrequent bowel movements.
2. Extraintestinal Symptoms
Celiac disease can also affect various organ systems outside the gastrointestinal tract, leading to extraintestinal symptoms such as:
- Fatigue: Persistent tiredness, weakness, or lack of energy, often unrelated to physical exertion.
- Weight Loss: Unintentional or unexplained weight loss despite adequate food intake.
- Anemia: Low red blood cell count, resulting in symptoms such as weakness, fatigue, and shortness of breath.
- Joint Pain: Pain, stiffness, or inflammation in the joints, resembling symptoms of arthritis.
- Infertility: Difficulty conceiving or carrying a pregnancy to term, particularly in women.
- Neurological Symptoms: Various neurological manifestations, including headaches, numbness or tingling in the extremities, balance problems, and cognitive impairment.
3. Dermatological Manifestations
Dermatological symptoms are common in celiac disease and may include:
- Dermatitis Herpetiformis: A chronic skin rash characterized by itchy, blistering lesions, typically occurring on the elbows, knees, buttocks, and scalp.
- Dry Skin: Rough, flaky, or excessively dry skin, often accompanied by itching or irritation.
- Skin Lesions: Other skin abnormalities, such as eczema, psoriasis, or chronic hives, may occur in some individuals with celiac disease.
4. Growth and Developmental Issues
Children with celiac disease may experience growth and developmental delays, including:
- Failure to Thrive: Inadequate weight gain or growth in infants and young children despite adequate caloric intake.
- Delayed Puberty: Late onset of puberty or delayed sexual development in adolescents.
5. Behavioral and Psychological Symptoms
Celiac disease can also affect mental health and well-being, leading to:
- Depression: Persistent feelings of sadness, hopelessness, or loss of interest in previously enjoyable activities.
- Anxiety: Excessive worry, fear, or nervousness, often accompanied by physical symptoms such as rapid heartbeat or sweating.
- Irritability: Increased irritability, mood swings, or emotional instability, particularly in children and adolescents.
6. Bone Health Complications
Inadequate absorption of nutrients, particularly calcium and vitamin D, in celiac disease can lead to:
- Osteoporosis: Weak, brittle bones with increased risk of fractures due to decreased bone density.
- Osteopenia: Reduced bone mineral density, a precursor to osteoporosis, often detected on bone density scans.
7. Dental Issues
Dental abnormalities may also occur in celiac disease, including:
- Dental Enamel Defects: Abnormalities in tooth enamel formation, resulting in discoloration, pitting, or grooving of the teeth.
- Delayed Tooth Eruption: Delayed or abnormal eruption of permanent teeth in children with celiac disease.
What is Gluten Sensitivity?
Distinction from Celiac Disease
Gluten sensitivity, also known as non-celiac gluten sensitivity, shares symptoms with celiac disease but does not involve the same autoimmune response or intestinal damage. Individuals with gluten sensitivity experience gastrointestinal symptoms after consuming gluten-containing foods.
Lack of Autoimmune Component
Unlike celiac disease, gluten sensitivity does not have an autoimmune component and does not cause long-term damage to the small intestine. However, it can still significantly impact quality of life and requires dietary management.
Gluten Containing Foods:
Gluten is found in various foods and ingredients, posing a challenge for individuals with celiac disease or gluten sensitivity. Understanding which foods contain gluten is essential for managing these conditions effectively.
1. Common Sources of Gluten
Gluten is naturally present in several grains and their derivatives, including:
- Wheat: The most well-known source of gluten, wheat is found in many foods and food products, both in its whole form and as processed ingredients.
- Barley: Barley and its products contain gluten, making them unsuitable for individuals on a gluten-free diet.
- Rye: Rye is another gluten-containing grain commonly used in bread, cereals, and other baked goods.
2. Products Derived from Gluten-Containing Grains
Gluten can also be found in various products derived from gluten-containing grains, including:
- Bread and Bakery Products: Wheat flour is a staple ingredient in bread, rolls, bagels, pastries, and other bakery items, all of which contain gluten.
- Pasta: Most traditional pasta products are made from wheat flour, making them off-limits for individuals avoiding gluten.
- Cereals: Many breakfast cereals contain wheat, barley, or rye as primary ingredients, contributing to their gluten content.
- Beer and Malt Beverages: Beer is typically brewed from barley, which contains gluten. Malt beverages and certain alcoholic drinks may also contain gluten-containing ingredients.
3. Processed Foods with Hidden Gluten
In addition to obvious sources, gluten can hide in various processed foods and food products, including:
- Sauces and Condiments: Soy sauce, teriyaki sauce, Worcestershire sauce, and certain salad dressings may contain gluten as a thickening agent or flavor enhancer.
- Processed Meats: Some processed meats, such as sausages, hot dogs, deli meats, and meatballs, may contain gluten-containing fillers or additives.
- Snack Foods: Many snack foods, including pretzels, crackers, chips, and flavored popcorn, may contain gluten in their seasoning blends or as a binding agent.
- Soups and Broths: Certain canned or packaged soups, broths, and bouillons may contain gluten as a thickener or stabilizer.
- Desserts and Sweets: Desserts such as cakes, cookies, pastries, and candies often contain wheat flour as a primary ingredient, contributing to their gluten content.
4. Cross-Contamination Risks
Cross-contamination can occur when gluten-free foods come into contact with gluten-containing ingredients or surfaces. Common sources of cross-contamination include:
- Shared Kitchen Utensils: Cutting boards, knives, toasters, and other kitchen utensils used for gluten-containing foods may transfer gluten particles to gluten-free foods.
- Bulk Bin Items: Bulk bin items, such as grains, flours, nuts, and spices, may become contaminated with gluten if they are stored or handled near gluten-containing products.
- Restaurant Dining: Restaurants and food service establishments may use shared cooking equipment or preparation surfaces, increasing the risk of cross-contamination for gluten-free menu items.
By identifying common sources of gluten and being mindful of potential cross-contamination risks, individuals following a gluten-free diet can make informed choices to protect their health and well-being.
Treatment of Celiac Disease:
Managing celiac disease involves a multifaceted approach that focuses on eliminating gluten from the diet, addressing nutritional deficiencies, and monitoring for complications. Here’s a detailed overview:
1. Gluten-Free Diet
The cornerstone of celiac disease treatment is strict adherence to a gluten-free diet. This involves avoiding all foods and products that contain gluten, including:
- Wheat: All varieties of wheat, including durum, semolina, spelt, and farro.
- Barley: Barley and its products, such as malt, malt extract, and malt vinegar.
- Rye: Rye and its derivatives, including rye flour and rye bread.
2. Gluten-Free Alternatives
Individuals with celiac disease can safely consume a wide range of naturally gluten-free foods, including:
- Fruits and Vegetables: Fresh fruits and vegetables are naturally gluten-free and provide essential vitamins, minerals, and fiber.
- Meat and Fish: Unprocessed meats and fish are naturally gluten-free and serve as excellent sources of protein.
- Dairy Products: Most dairy products, such as milk, cheese, and yogurt, are gluten-free, although flavored varieties should be checked for additives.
- Gluten-Free Grains: Gluten-free grains like rice, corn, quinoa, millet, and buckwheat can be enjoyed as alternatives to wheat, barley, and rye.
3. Gluten-Free Label Reading
Learning to read food labels is essential for individuals with celiac disease to identify gluten-containing ingredients and avoid cross-contamination. Look for gluten-free certification labels and be vigilant about hidden sources of gluten in processed foods.
4. Nutritional Support
Malabsorption of nutrients due to intestinal damage in celiac disease can lead to nutritional deficiencies. Nutritional support may include:
- Vitamin and Mineral Supplements: Individuals with celiac disease may require supplements to address deficiencies in vitamins and minerals such as iron, calcium, vitamin D, vitamin B12, and folate.
- Probiotics: Probiotic supplements may help restore gut microbiota balance and support digestive health in individuals with celiac disease.
5. Follow-Up Care
Regular follow-up care with a healthcare provider is essential for monitoring the progress of celiac disease treatment and addressing any ongoing concerns. Follow-up care may include:
- Periodic Blood Tests: Blood tests to monitor antibody levels and assess nutritional status, including iron levels and vitamin D levels.
- Intestinal Biopsy: In some cases, repeat intestinal biopsy may be performed to evaluate the healing of the intestinal lining and confirm adherence to a gluten-free diet.
- Consultation with Registered Dietitian: Working with a registered dietitian who specializes in celiac disease can provide personalized dietary guidance and support.
6. Support Groups and Resources
Joining support groups and accessing reputable resources can provide valuable support and information for individuals living with celiac disease. These resources may include:
- Celiac Disease Support Groups: Local or online support groups can connect individuals with others who understand the challenges of living with celiac disease and provide practical tips and advice.
- Educational Materials: Accessing educational materials, books, websites, and reputable organizations dedicated to celiac disease can help individuals stay informed and empowered to manage their condition effectively.
By following a gluten-free diet, addressing nutritional deficiencies, and receiving ongoing medical care and support, individuals with celiac disease can lead healthy, fulfilling lives while effectively managing their condition.
Prevention:
Early Detection
While celiac disease cannot be prevented, early detection and diagnosis can help prevent complications and improve outcomes. Screening individuals with a family history of celiac disease or related autoimmune conditions may help identify those at risk.
Genetic Testing
Genetic testing for the HLA-DQ2 and HLA-DQ8 genes may be recommended for family members of individuals with celiac disease. Identifying genetic susceptibility can guide early intervention and dietary management.
Differential Diagnosis:
Differential diagnosis involves distinguishing celiacs disease from other gastrointestinal disorders with similar symptoms, such as irritable bowel syndrome, Crohn’s disease, and lactose intolerance. This may require a combination of blood tests, intestinal biopsy, and dietary elimination trials to accurately diagnose celiac disease and develop an appropriate treatment plan.
Read Another Article: Health Benefits of Aparijita


Pingback: Gluten Sensitivity: Foods to Avoid - Modern Health
Pingback: Gluten sensitivity foods to avoid - AcconstHost
Pingback: Foods to avoid in gluten sensitivity - ECG Oxford
Pingback: foods to avoid in gluten sensitivity - MedWebMD