History:
A 16-year-old male presents with a history of persistent high blood pressure, despite being on multiple antihypertensive medications. Additionally, he reports episodes of muscle weakness and fatigue. No significant family history of hypertension or renal disease is noted, making this case intriguing.
Examination:
General Examination
- General Condition (GC): Alert and oriented.
- Pulse: 82 beats per minute, regular.
- Blood Pressure (BP): Consistently above 150/90 mm Hg.
- Respiratory Rate (RR): 16 breaths per minute.
- SpO2: 98% on room air.
- Pallor: Absent.
- Icterus: Absent.
- Cyanosis: Absent.
- Lymphadenopathy: Absent.
- Edema: Absent.
Systemic Examination
- Respiratory System (RS): Clear breath sounds bilaterally, no wheezes or crackles.
- Cardiovascular System (CVS):
- Normal heart sounds, no murmurs.
- Elevated blood pressure without postural hypotension.
- Per Abdomen (PA):
- Soft and non-tender.
- No organomegaly or palpable masses.
- Central Nervous System (CNS):
- Normal muscle tone and strength.
- Reflexes are normal, but slight muscle weakness in the lower extremities is noted.
Diagnostic Evaluation
Laboratory Findings
Complete Blood Count (CBC)
- Hemoglobin (Hb): 14.0 g/dL (normal range: 13.8-17.2 g/dL).
- White Blood Cell Count (WBC): 7,000 cells/μL (normal range: 4,500-11,000 cells/μL).
- Platelet Count: 250,000 cells/μL (normal range: 150,000-450,000 cells/μL).
- Hematocrit (Hct): 42% (normal range: 38-50%).
- Mean Corpuscular Volume (MCV): 88 fL (normal range: 80-100 fL).
Liver Function Tests (LFT) and Renal Function Tests (RFT)
- Alanine Aminotransferase (ALT): 22 IU/L (normal range: 7-56 IU/L).
- Aspartate Aminotransferase (AST): 20 IU/L (normal range: 10-40 IU/L).
- Alkaline Phosphatase (ALP): 70 IU/L (normal range: 44-147 IU/L).
- Total Bilirubin: 0.8 mg/dL (normal range: 0.1-1.2 mg/dL).
- Blood Urea Nitrogen (BUN): 14 mg/dL (normal range: 7-20 mg/dL).
- Serum Creatinine: 0.8 mg/dL (normal range: 0.6-1.2 mg/dL).
Electrolytes and Other Relevant Tests
- Serum Sodium: 145 mEq/L (normal range: 135-145 mEq/L).
- Serum Potassium: 2.8 mEq/L (normal range: 3.5-5.0 mEq/L) – indicating hypokalemia.
- Serum Bicarbonate: 30 mEq/L (normal range: 22-28 mEq/L) – indicating metabolic alkalosis.
- Serum Chloride: 97 mEq/L (normal range: 96-106 mEq/L).
- Renin Activity: Suppressed (<0.6 ng/mL/hr).
- Aldosterone Level: Low (2 ng/dL, normal range: 4-15 ng/dL).
- Urinary Potassium Excretion: Elevated at 80 mEq/day (normal range: 25-125 mEq/day).
Arterial Blood Gas (ABG)
- pH: 7.48 (normal range: 7.35-7.45) – indicating alkalosis.
- PaCO2: 38 mm Hg (normal range: 35-45 mm Hg).
- PaO2: 95 mm Hg (normal range: 75-100 mm Hg).
- HCO3-: 30 mEq/L (normal range: 22-28 mEq/L) – confirming metabolic alkalosis.
Thyroid Function Tests (TFT)
- Thyroid-Stimulating Hormone (TSH): 2.0 mIU/L (normal range: 0.4-4.0 mIU/L).
- Free T4 (Thyroxine): 1.2 ng/dL (normal range: 0.8-2.0 ng/dL).
- Free T3 (Triiodothyronine): 3.1 pg/mL (normal range: 2.3-4.2 pg/mL).
Additional Endocrine Tests
To rule out other endocrine causes of hypertension, the following tests were conducted:
- 24-Hour Urinary Free Cortisol: 40 µg/day (normal range: 20-90 µg/day) – to rule out Cushing’s syndrome.
- Plasma Metanephrines: Normal levels, to rule out pheochromocytoma.
- Dexamethasone Suppression Test: Normal cortisol suppression, further ruling out Cushing’s syndrome.
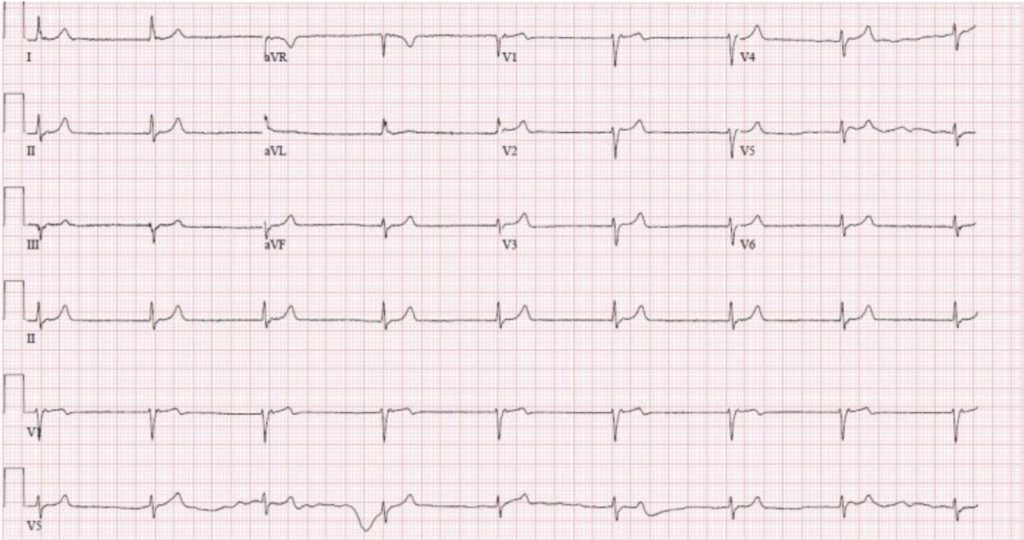
Electrocardiogram (ECG)
- ECG Findings:
- Sinus rhythm.
- Slightly prolonged QT interval.
- U waves visible, consistent with hypokalemia.
Radiological Investigations
To rule out other potential causes of secondary hypertension, several radiological investigations were performed:
- Ultrasound Abdomen and Pelvis (USG A+P):
- Kidneys of normal size and echotexture.
- No evidence of hydronephrosis or renal masses.
- Normal adrenal glands, ruling out adrenal pathology.
- Renal Artery Doppler:
- No evidence of renal artery stenosis or other vascular abnormalities.
- Normal blood flow velocities in renal arteries.
- Renal Angiogram:
- Confirmed the absence of renal artery stenosis or other vascular abnormalities.
- Excluded fibromuscular dysplasia, which can also cause secondary hypertension.
Additional Tests
- Genetic Testing: Confirmed mutations in the SCNN1B or SCNN1G genes, encoding the epithelial sodium channel (ENaC), confirming the diagnosis of Liddle syndrome.
Diagnosis
The combination of clinical features, laboratory findings, and radiological investigations strongly suggests Liddle syndrome. Genetic testing confirms the diagnosis by identifying mutations in the SCNN1B or SCNN1G genes, which encode the epithelial sodium channel (ENaC). These mutations result in increased sodium reabsorption and potassium excretion, leading to hypertension and hypokalemia.
Pathophysiology
Liddle syndrome arises from mutations in genes encoding subunits of the epithelial sodium channel (ENaC) in the distal renal tubules. These mutations cause the channels to remain open longer than normal, increasing sodium reabsorption and potassium excretion. Consequently, patients exhibit:
- Hypertension: Due to increased sodium and water retention.
- Hypokalemia: Due to excessive potassium excretion.
Clinical Features
Liddle syndrome presents with:
- Severe Hypertension: Often resistant to standard antihypertensive treatments.
- Hypokalemia: Leading to symptoms like muscle weakness, fatigue, and cardiac arrhythmias.
- Metabolic Alkalosis: Due to excessive potassium loss.
Management
Medications
Treating Liddle syndrome primarily involves:
- Potassium-Sparing Diuretics: Such as amiloride or triamterene, which directly inhibit ENaC.
- Antihypertensive Agents: Beta-blockers, calcium channel blockers, or ACE inhibitors may be used adjunctively.
Lifestyle Modifications
Patients are advised to:
- Adopt a Low-Sodium Diet: To minimize sodium reabsorption.
- Monitor Potassium Levels: Regularly, to prevent hypokalemia.
Conclusion
Liddle syndrome, though rare, is a critical diagnosis to consider in cases of resistant hypertension and hypokalemia. Early recognition and appropriate management can significantly improve patient outcomes.