History
A 35-year-old male with a history of HIV/AIDS presents to the emergency department with progressive shortness of breath, non-productive cough, and fever over the past two weeks. The patient reports significant weight loss and night sweats over the last three months. He has not been adherent to his antiretroviral therapy.
Examination
General Examination
- Appearance: The patient appears cachectic and in mild respiratory distress.
- Vital Signs:
- Temperature: 101°F (38.3°C), indicating fever.
- Blood Pressure: 110/70 mmHg, normal.
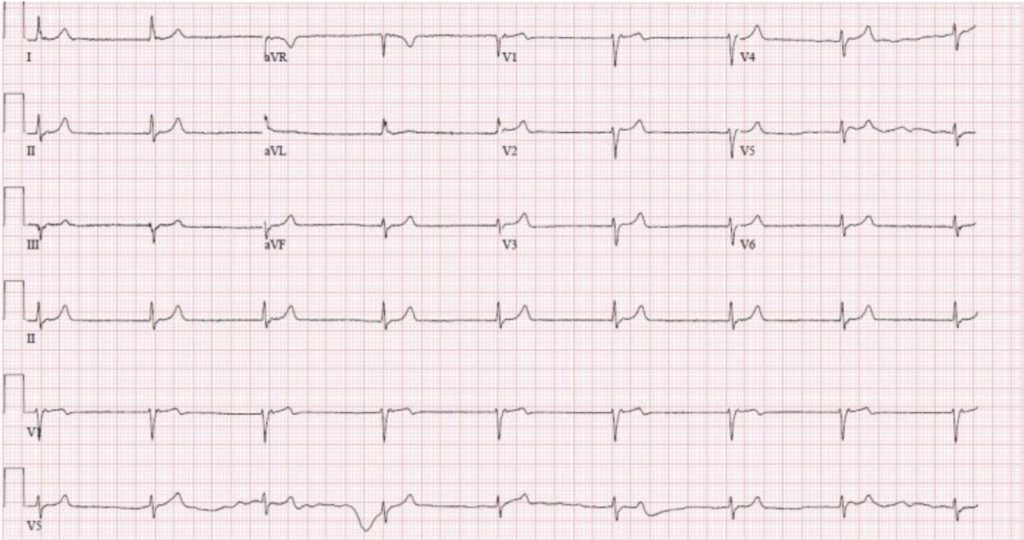
- Heart Rate: 105 beats per minute, elevated.
- Respiratory Rate: 28 breaths per minute, elevated.
- Oxygen Saturation: 88% on room air, decreased.
Respiratory Examination
- Inspection: Increased work of breathing with use of accessory muscles.
- Auscultation: Bilateral crackles (rales) predominantly in the lower lung fields.
- Percussion: Dullness over lung bases.
- Palpation: Reduced chest expansion bilaterally.
Diagnostic Workup
Blood Tests
- Complete Blood Count (CBC): Elevated white blood cell count indicating infection.
- Arterial Blood Gas (ABG): Hypoxemia with a PaO2 of 60 mmHg and respiratory alkalosis.
- CD4 Count: Below 200 cells/µL, confirming severe immunosuppression.
Imaging
- Chest X-ray: Bilateral interstitial infiltrates, often described as “ground-glass” opacities.

- High-Resolution CT (HRCT): Diffuse ground-glass opacities with a “crazy paving” pattern.
Microbiological Tests
- Induced Sputum or Bronchoalveolar Lavage (BAL): Staining (Giemsa or methenamine silver) identifies cysts and trophozoites of Pneumocystis jirovecii (formerly Pneumocystis carinii).
Other Tests
- Lactate Dehydrogenase (LDH): Elevated levels are often seen in PCP and can help support the diagnosis.
Overview:
Pneumocystis carinii pneumonia (PCP) is a serious fungal infection primarily affecting immunocompromised individuals.
Pathophysiology
PCP is caused by the fungus Pneumocystis jirovecii. This organism primarily affects the alveoli in the lungs, leading to:
- Alveolar Infiltration: The fungus fills the alveoli, causing impaired gas exchange.
- Inflammatory Response: The host’s immune response leads to further lung damage and symptoms.
- Hypoxemia: Due to impaired oxygen exchange, patients experience significant hypoxemia.
Management:
Initial Management
- Oxygen Therapy: Administer supplemental oxygen to maintain adequate oxygen saturation.
- Antimicrobial Therapy: Start high-dose trimethoprim-sulfamethoxazole (TMP-SMX) as the first-line treatment.
- Corticosteroids: For patients with moderate to severe PCP (PaO2 <70 mmHg or A-a gradient >35 mmHg), adjunctive corticosteroids reduce inflammation and improve outcomes.
Monitoring and Supportive Care
- Regular Monitoring: Frequent assessment of respiratory status, oxygenation, and response to therapy.
- Hydration and Nutrition: Ensure adequate fluid intake and nutritional support.
- Management of Complications: Be vigilant for complications such as pneumothorax and acute respiratory distress syndrome (ARDS).
Prevention
- Prophylaxis: HIV patients with CD4 counts below 200 cells/µL should receive PCP prophylaxis with TMP-SMX or an alternative such as dapsone or atovaquone.
- Adherence to Antiretroviral Therapy: Ensure patients with HIV are adherent to their antiretroviral therapy to maintain immune function.
Conclusion
Pneumocystis carinii pneumonia (PCP) remains a significant opportunistic infection in immunocompromised individuals, particularly those with HIV/AIDS. Prompt recognition, appropriate diagnostic workup, and timely initiation of treatment are crucial for improving patient outcomes. Preventive measures, including prophylaxis and adherence to antiretroviral therapy, play a vital role in reducing the incidence of PCP.