
Acute paralysis by hypokalemia;
Case presentation:
A 58 year old male presented with complaints of 10-12 episodes of vomitting. His was vitally stable. Signs of dehydration were present. He was admitted, and was later complaining of inability to move his legs and was not able to lift his neck up.
Detail examination findings:
- Pulse – 84/Min, Regular
- Blood pressure- 90/70 mmHg
- Resp. Rate – 16/min
- Spo2 – 97% (Off O2, On room Air)
- Afebrile
- signs of Dehydration present
Systemic Examination:
- CVS- S1S2 – Normal, No Murmur
- RS- Air Entry Bilaterally Equal, No added Sounds
- Per Abdo – Soft, Non Tender, No Distension
- CNS- Conscious, Oriented to Time, person & place.
- Tone – Reduced in all four limbs
- Deep Tendon Reflexes – Exaggerated in lower limbs
- Plantars – B/L Flexors
- Pupils – B/L Normal sized, Reacting to Light
- Neck Hold – Poor/ Not able to lift & hold neck.
- No muscle fasciculations present
Laboratory Findings :
- Hemoglobin (Hb): Actual Value: [14.3] g/dL
- Normal Range: Male: 13.8 to 17.2 grams per deciliter (g/dL); Female: 12.1 to 15.1 g/dL.
- White Blood Cell Count (WBC):
- Actual Count: [12,400] cells/μL
- Normal Range: 4,500 to 11,000 cells per microliter (cells/μL)
- Actual Count: [12,400] cells/μL
- Platelet Count:
- Actual Count: [200000] platelets/μL
- Normal Range: 150,000 to 450,000 platelets per microliter (platelets/μL)
- Actual Count: [200000] platelets/μL
- Red Blood Cell Count (RBC):
- Actual Count: [4.9] million cells/μL
- Normal Range: Male: 4.7 to 6.1 million cells/μL; Female: 4.2 to 5.4 million cells/μL
- Actual Count: [4.9] million cells/μL
- Hematocrit (Hct):
- Actual Value: [45] %
- Normal Range: Male: 40.7% to 50.3%; Female: 36.1% to 44.3%
- Actual Value: [45] %
- Mean Corpuscular Volume (MCV):
- Actual Value: [82] fL
- Normal Range: 80 to 96 femtoliters (fL)
- Actual Value: [82] fL
- Mean Corpuscular Hemoglobin (MCH):
- Actual Value: [30] pg
- Normal Range: 27 to 31 picograms (pg)
- Actual Value: [30] pg
- Mean Corpuscular Hemoglobin Concentration (MCHC):
- Actual Value: [33] g/dL
- Normal Range: 32 to 36 grams per deciliter (g/dL)
- Actual Value: [33] g/dL
Liver Function Test (LFT):
- Total Bilirubin: [1.7] mg/dL
- AST: [54] IU/L
- ALT: [47] IU/L
- ALP: [112] IU/L
Kidney Function Test (KFT):
- BUN: [45] mg/dL
- Creatinine: [2.2] mg/dL
- Sodium (Na+): [137] mEq/L
- Potassium (K+) : [1.72] mEq/L
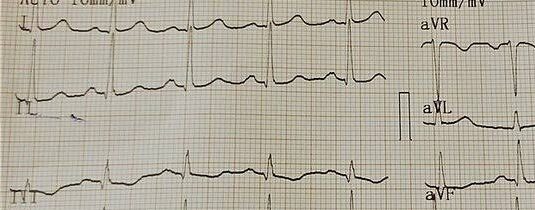
ECG:
What’s the diagnosis?
After clinically evaluating the patient and carefully looking at the lab values, we obviously found some abnormal values like:
- Serum Creatinine- 2.2 mg/dL
- Serum Potassium (K+) – 1.72 mEq/L
- Hypovolemia
- Ecg findings suggestive of Hypokalemia
- Clinical findings like muscle weakness
Our team had DDS that were close ones:
- GBS
- Hypokalemia Induced Weakness/Paralysis
Patient gave history of acute weakness of all four limbs and neck. There was no typical presentation of ascending or descending muscle weakness. He felt muscle weakness in all at same time.
His bladder and bowel was intact, No BB involvement was there. There was no respiratory muscle involvement (No SOB, or Dyspnea) .
Patients Response to Treatment:
After replenishment of intravascular fluids volume and giving supportive treatment his blood pressure was back to normal range.
Response Potassium replacement:
Patients complain of muscle weakness and inability to hold his neck was improving as potassium replacement was started.
Patients urine output was normal since admission.
Potassium and other electrolytes can be lost through GI tract and can lead to serious health issues. Let’s see how GI tract losses potassium:
Potassium loss in Gastrointestinal track:
In acute gastroenteritis, potassium losses through the gastrointestinal (GI) tract can be significant due to vomiting and diarrhea, which are common symptoms of the condition. Here’s how potassium losses in the GI tract may occur in acute gastroenteritis:
- Vomiting:
- Persistent vomiting can lead to the loss of stomach contents, including potassium-rich gastric juices.
- This can result in rapid depletion of potassium levels in the body.
- Diarrhea:
- Diarrhea in gastroenteritis causes fluid and electrolyte losses, including potassium.
- The rapid transit of stool through the intestines limits the absorption of nutrients, including potassium, leading to further losses.
- Increased GI Motility:
- In acute gastroenteritis, the GI tract may experience increased motility, reducing the time available for nutrient absorption, including potassium.
- This can exacerbate potassium losses, particularly in severe cases of diarrhea.
- Dehydration:
- Fluid loss through vomiting and diarrhea can lead to dehydration, which further concentrates electrolytes in the remaining body fluids, including potassium.
- Dehydration can exacerbate electrolyte imbalances, potentially leading to complications such as muscle weakness, cardiac arrhythmias, or even cardiac arrest in severe cases.
Managing potassium losses in acute gastroenteritis involves fluid and electrolyte replacement, either orally or intravenously, depending on the severity of symptoms. Rehydration solutions containing electrolytes, including potassium, are often used to restore fluid and electrolyte balance in affected individuals. However, it’s essential to monitor potassium levels closely, especially in severe cases, to prevent complications associated with electrolyte imbalances.
How does Hypokalemia causes paralysis?
Hypokalemia, which is low potassium levels in the blood, can lead to muscle weakness and even paralysis. Here’s how hypokalemia causes paralysis:
- Impaired Muscle Function: Potassium is essential for normal muscle function, including muscle contraction and relaxation. When potassium levels are low, the ability of muscles to contract properly is compromised.
- Altered Membrane Potential: Potassium plays a crucial role in maintaining the resting membrane potential of muscle cells. In hypokalemia, there is a decreased concentration of potassium ions inside the cell, which disrupts the balance of ions across the cell membrane. This alteration in membrane potential affects the excitability of muscle cells, leading to impaired muscle function.
- Impaired Neuromuscular Transmission: Potassium is involved in the transmission of nerve impulses to muscles. In hypokalemia, reduced potassium levels can interfere with the transmission of signals from nerves to muscles, resulting in weakness and potentially paralysis.
- Muscle Fatigue and Weakness: As hypokalemia progresses, muscle fatigue and weakness become more pronounced. This weakness can eventually lead to paralysis, where muscles lose their ability to contract altogether.
- Respiratory and Cardiac Muscle Involvement: Severe hypokalemia can affect not only skeletal muscles but also respiratory muscles (diaphragm) and cardiac muscles. Paralysis of respiratory muscles can lead to respiratory failure, while cardiac muscle dysfunction can result in life-threatening arrhythmias.
In summary, hypokalemia-induced paralysis occurs due to impaired muscle function, altered membrane potential, disrupted neuromuscular transmission, and eventual muscle fatigue and weakness.
How to treat Hypokalemia?
Treating hypokalemia involves replenishing potassium levels in the body and addressing any underlying causes contributing to the low potassium levels. Here are common treatment approaches:
- Oral Potassium Supplements: Mild to moderate cases of hypokalemia can often be treated with oral potassium supplements. These supplements come in various forms, including potassium chloride tablets or solutions. They should be taken as prescribed by a healthcare professional, typically with food to minimize gastrointestinal irritation.
- Intravenous (IV) Potassium: Severe cases of hypokalemia or situations where oral supplementation is not feasible (e.g., vomiting, ileus) may require intravenous potassium administration. IV potassium should be administered cautiously and under close medical supervision to avoid the risk of complications such as cardiac arrhythmias.
- Addressing Underlying Causes: It’s essential to identify and address any underlying factors contributing to hypokalemia. This may include adjusting medications that promote potassium loss (e.g., diuretics), treating conditions such as diarrhea or vomiting, or addressing hormonal imbalances (e.g., hyperaldosteronism).
- Dietary Changes: In addition to supplementation, increasing dietary potassium intake can help prevent recurrence of hypokalemia. Foods rich in potassium include bananas, oranges, potatoes, tomatoes, spinach, avocados, and beans. However, dietary modifications alone may not be sufficient to correct severe hypokalemia.
- Monitoring and Follow-up: Regular monitoring of potassium levels is essential during treatment to ensure that levels return to normal without causing hyperkalemia (high potassium levels). Follow-up appointments with healthcare providers are important to assess treatment efficacy and address any ongoing potassium imbalances.
- Correction of Magnesium Deficiency: Hypokalemia may be associated with magnesium deficiency, as magnesium is necessary for potassium reabsorption in the kidneys. Therefore, correcting concurrent magnesium deficiency may help improve potassium levels.
It’s crucial to manage hypokalemia under the guidance of a healthcare professional, as improper treatment or correction of potassium levels can lead to serious complications, including cardiac arrhythmias. Treatment should be individualized based on the severity of hypokalemia, the presence of underlying conditions, and other patient-specific factors.
Read more:

