End organ damage due to Hypertension;
Overview:
End organ damage, often abbreviated as EOD, refers to the irreversible harm inflicted on vital organs as a result of various medical conditions or lifestyle factors.
- Overview:
- what is Hypertension-Induced End Organ Damage?
- How to access End organ Damage?
- Hypertensive Nephropathy – Kidney Damage:
- Hypertensive Heart Disease:
- Signs and Symptoms of Hypertension-Induced End Organ Damage
- • Diabetes:
- Diabetes-Induced End Organ Damage:
- Atherosclerosis: A Silent Threat
- Chronic Inflammation and End Organ Damage
- Lifestyle Factors and End Organ Damage
- Consequences of End Organ Damage
- References:
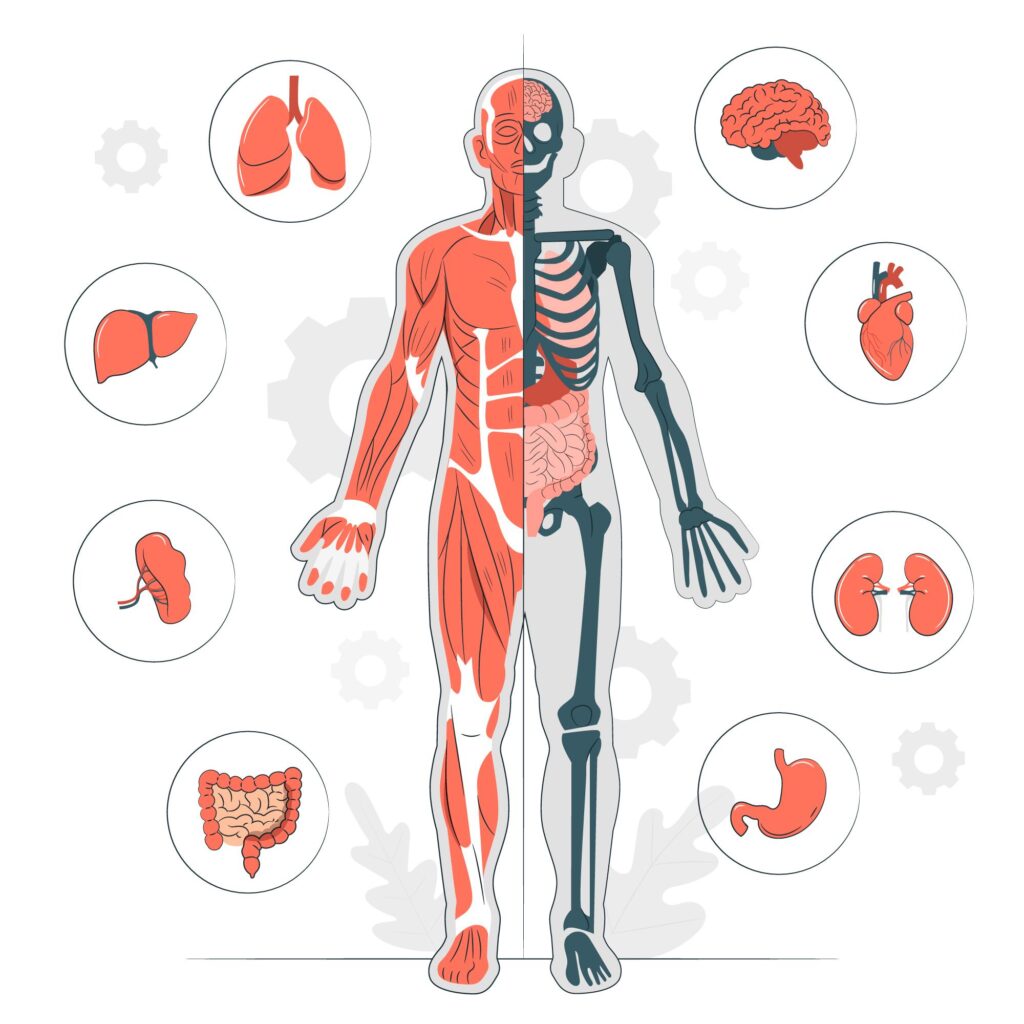
End organ damage is a serious consequence of conditions like hypertension and diabetes.
what is Hypertension-Induced End Organ Damage?
Hypertension-induced end organ damage refers to the progressive deterioration of vital organs resulting from chronic high blood pressure. Prolonged elevation in blood pressure levels places excessive strain on the arteries, leading to structural and functional abnormalities in organs such as the heart, kidneys, brain, and blood vessels.
How to access End organ Damage?
1. Hypertensive Vasculopathy:
Measurement of the intima-media thickness in the common carotid artery and of the pulse-wave velocity is now recommended for the early diagnosis of hypertensive vasculopathy.
2. Hypertensive Heart Disease:
Left ventricular hypertrophy, an important component of hypertensive heart disease, can be diagnosed by echocardiography – (2D Echo) and with the aid of new electrocardiographic indices.
3. Hypertensive Nephropathy :
Early signs of hypertensive nephropathy, namely albuminuria and a decreased glomerular filtration rate (Reduced eGFR) , are prognostically valuable and easy to detect.
4. Cerebrovascular Damage:
Cerebrovascular damage, including early microangiopathic changes, is best diagnosed by magnetic resonance imaging. The treatment of end organ damage due to hypertension centers on blood pressure reduction. Blockade of the renin angiotensin-aldosterone system is an essential part of the treatment of early end organ damage.
Hypertensive Nephropathy – Kidney Damage:
Hypertensive nephropathy often leads to chronic renal failure after 15 to 20 years, typically without noticeable symptoms.
Early Detection:
- Identifying Albuminuria and Reduced eGFR
- Early signs include mild albuminuria and decreased glomerular filtration rate (eGFR), easily measurable parameters
Prevention:
Rigorous antihypertensive therapy with ACE Inhibitors (Nephroprotective Effects), ARB’s or direct renine inhibitors, mostly in multiple combinations with Diuretics and calcium antagonists, can prevent the progression of chronic renal failure and proteinuria and thereby improve both the renal and cardiovascular prognosis.
Target Blood pressure:
Recommended target blood pressure of <130/80 mm Hg In hypertensive nephropathy and in the presence of proteinuria the blood pressure should be even lower
Hypertensive Heart Disease:
Hypertensive heart disease encompasses a range of functional and structural cardiac alterations. Left ventricular hypertrophy (LVH) is a key aspect. Typically asymptomatic, hypertensive heart disease may present in advanced stages as angina pectoris, dyspnea, and arrhythmia. These symptoms stem from reduced coronary reserve, compromised systolic and diastolic left ventricular function, atrial fibrillation, and ventricular arrhythmia.
Therefore, in addition to coronary heart disease, the presence of angina should also prompt consideration of hypertensive heart disease. Furthermore, even in early stages, a diastolic filling disorder may arise due to delayed left ventricular relaxation.
In advanced stages, reduced left ventricular compliance develops, potentially leading to diastolic heart failure.
How to Diagnose?
Echocardiography (2D echo) is the gold standard for diagnosing hypertensive heart disease, But ECG is more commonly used. 2D echo will tell you about dimensions of heart chambers.
Prognosis of Hypertensive Heart Disease (LVH):
Left ventricular hypertrophy elevates the risk of myocardial infarction, heart failure, and sudden cardiac death by three to five times. Concentric hypertrophy (relative wall thickness ≥ 0.42) leads to a poorer cardiovascular prognosis.
Treatment:
Treatment for left ventricular hypertrophy has demonstrated that inhibitors of the renin-angiotensin system and calcium antagonists reduce left ventricular mass beyond blood pressure reduction alone. Reducing left ventricular mass decreases the risk of cardiovascular events by over half.
ACE inhibitors and angiotensin receptor blockers (ARB’s) are the preferred agents for primary prevention of atrial fibrillation, surpassing beta blockers, which are favored for controlling heart rate in absolute tachyarrhythmia.
➡️ Read Another Article: Myocardial Infarction
Myocardial Infarction – Types, ECG Changes And Culprit Vessels
Signs and Symptoms of Hypertension-Induced End Organ Damage
The signs and symptoms of hypertension-induced end organ damage vary depending on the affected organ:
- Heart: Symptoms may include chest pain (angina), shortness of breath, fatigue, and palpitations.
- Kidneys: Individuals may experience changes in urinary frequency, fluid retention, swelling in the legs or abdomen, and elevated blood pressure.
- Brain: Symptoms can manifest as headaches, dizziness, visual disturbances, confusion, and transient ischemic attacks (TIAs) or strokes.
- Blood Vessels: Complications may include peripheral arterial disease (PAD), manifested by leg pain during walking, and an increased risk of aneurysm formation.
Treatment :
Management of hypertension-induced end organ damage primarily revolves around controlling blood pressure levels and addressing associated complications. Treatment modalities may include:
- Antihypertensive Medications: Pharmacological agents such as ACE inhibitors, angiotensin II receptor blockers (ARBs), beta-blockers, calcium channel blockers, and diuretics are commonly prescribed to lower blood pressure and mitigate end organ damage.
- Lifestyle Modifications: Encouraging lifestyle changes such as adopting a heart-healthy diet, engaging in regular physical activity, limiting alcohol intake, quitting smoking, and reducing stress can complement pharmacotherapy and improve overall cardiovascular health.
Prevention Measures
Preventing hypertension-induced end organ damage requires a multifaceted approach aimed at reducing modifiable risk factors and promoting cardiovascular health:
- Regular Blood Pressure Monitoring: Periodic assessment of blood pressure levels enables early detection and intervention to prevent end organ damage.
- Healthy Lifestyle Habits: Emphasizing the importance of maintaining a balanced diet rich in fruits, vegetables, and whole grains, engaging in regular exercise, maintaining a healthy weight, and managing stress can help prevent hypertension and its sequelae.
- Compliance with Medical Treatment: Adherence to prescribed antihypertensive medications and routine follow-up visits with healthcare providers are essential for optimizing blood pressure control and minimizing the risk of end organ damage.
Potential Complications
Failure to adequately manage hypertension-induced end organ damage can result in severe complications, including:
- Heart Failure: Chronic hypertension can lead to left ventricular hypertrophy, myocardial ischemia, and ultimately heart failure.
- Chronic Kidney Disease (CKD): Persistent elevation in blood pressure damages the kidneys’ delicate filtration units, leading to progressive decline in renal function and the development of CKD.
- Stroke: Hypertension is a major risk factor for ischemic and hemorrhagic strokes, which can result in significant neurological deficits or death if left untreated.
• Diabetes:
Chronic hyperglycemia in diabetes harms blood vessels and nerves, causing complications such as retinopathy, nephropathy, and neuropathy, accelerating atherosclerosis and worsening end organ damage.
Diabetes-Induced End Organ Damage:
Diabetes, a chronic metabolic disorder characterized by elevated blood glucose levels, poses a significant threat to various organs in the body through its insidious process of inducing end organ damage. In this article, we will delve into the definition, mechanisms, treatment, prevention, and potential complications of diabetes-induced end organ damage.
Defining Diabetes-Induced End Organ Damage
Diabetes-induced end organ damage refers to the progressive deterioration of vital organs resulting from chronic hyperglycemia. Prolonged exposure to elevated glucose levels wreaks havoc on blood vessels, nerves, and organs throughout the body, leading to structural and functional abnormalities in organs such as the eyes, kidneys, nerves, and cardiovascular system.
Mechanisms of Diabetes-Induced End Organ Damage
The mechanism underlying diabetes-induced end organ damage is multifactorial and involves several pathological processes:
- Advanced Glycation End Products (AGEs): Elevated glucose levels react with proteins to form AGEs, which accumulate in tissues and contribute to inflammation, oxidative stress, and tissue damage.
- Microvascular Complications: Chronic hyperglycemia damages small blood vessels, leading to microvascular complications such as retinopathy, nephropathy, and neuropathy.
- Macrovascular Complications: Diabetes accelerates the progression of atherosclerosis, increasing the risk of macrovascular complications such as coronary artery disease, peripheral arterial disease, and stroke.
Treatment Strategies
Management of diabetes-induced end organ damage focuses on controlling blood glucose levels and addressing associated complications. Treatment modalities may include:
- Glucose-Lowering Medications: Pharmacological agents such as insulin, oral hypoglycemic agents (e.g., metformin, sulfonylureas, SGLT2 inhibitors), and injectable medications (e.g., GLP-1 receptor agonists) are prescribed to lower blood glucose levels and mitigate end organ damage.
- Blood Pressure and Lipid Control: Tight control of blood pressure and lipid levels is essential for reducing the risk of cardiovascular complications in individuals with diabetes.
- Regular Screening and Monitoring: Routine screening for diabetes-related complications, including eye exams, urine tests for proteinuria, and nerve function tests, allows for early detection and intervention to prevent or delay the progression of end organ damage.
Prevention Measures
Preventing diabetes-induced end organ damage requires a comprehensive approach aimed at reducing modifiable risk factors and promoting overall health:
- Blood Glucose Management: Achieving and maintaining optimal blood glucose control through lifestyle modifications (e.g., healthy diet, regular exercise) and adherence to prescribed medications is crucial for preventing diabetes-related complications.
- Blood Pressure and Cholesterol Management: Controlling hypertension and dyslipidemia through lifestyle changes and medication therapy helps reduce the risk of cardiovascular complications in individuals with diabetes.
- Regular Medical Follow-Up: Regular visits to healthcare providers for monitoring and management of diabetes-related complications enable early detection and intervention to prevent or delay the progression of end organ damage.
Potential Complications
Failure to adequately manage diabetes-induced end organ damage can result in severe complications, including:
- Diabetic Retinopathy: Damage to the blood vessels in the retina can lead to vision loss and blindness.
- Diabetic Nephropathy: Damage to the kidneys’ filtration units can result in chronic kidney disease and end-stage renal disease.
- Diabetic Neuropathy: Nerve damage can cause sensory disturbances, pain, and loss of function in the extremities.
- Cardiovascular Disease: Diabetes significantly increases the risk of coronary artery disease, heart attack, stroke, and peripheral arterial disease.
Atherosclerosis: A Silent Threat
Atherosclerosis, characterized by the buildup of plaque within arterial walls, underlies numerous cases of end organ damage. The gradual accumulation of cholesterol, inflammatory cells, and fibrous tissue narrows the arteries, impeding blood flow to vital organs. Ultimately, this process can culminate in myocardial infarction, stroke, or peripheral vascular disease, depending on the affected arteries.
Chronic Inflammation and End Organ Damage
Chronic inflammation serves as a driving force behind end organ damage in various pathological conditions. Persistent inflammation within the body triggers a cascade of immune responses that contribute to tissue injury and dysfunction. Organs such as the liver, lungs, and joints may suffer irreparable harm as a result of prolonged inflammatory insults.
Lifestyle Factors and End Organ Damage
Beyond medical conditions, certain lifestyle factors can predispose individuals to end organ damage. Smoking, excessive alcohol consumption, sedentary behavior, and poor dietary habits all contribute to systemic inflammation, oxidative stress, and endothelial dysfunction. Over time, these behaviors exact a toll on vital organs, hastening the onset of end organ damage.
Consequences of End Organ Damage
The consequences of end organ damage are far-reaching and profound. Affected individuals may experience a decline in quality of life, debilitating symptoms, and increased morbidity and mortality rates. Heart failure, chronic kidney disease, stroke, and peripheral neuropathy are just a few examples of the debilitating conditions that can arise from untreated end organ damage.
References:
End organ damage. Science direct. https://www.sciencedirect.com/topics/medicine-and-dentistry/end-organ-damage
Accessed on 22-06-2022
- What end-organ damage may occur during a hypertensive emergency? MedScape. https://www.medscape.com/answers/241381-7577/what-end-organ-damage-may-occur-during-a-hypertensive-emergency
Accessed on 22-06-2022
- Creatinine clearance and signs of end-organ damage in primary hypertension. Journal of human hypertension. https://www.nature.com/articles/1001689
Accessed on 22-06-2022
- Genetics of Hypertension, Target-Organ Complications, and Response to Therapy. Circulation. American Heart Asociation. https://www.ahajournals.org/doi/10.1161/circ.102.suppl_4.IV-40


Pingback: End Organ Damage by Hypertension - Modern Health
Pingback: Diabetes Mellitus: Types, Causes, Symptoms, and Treatment - Modern Health
Pingback: Hypertension and its Impact on End-Organ Damage -Review - Modern Health
Pingback: - Acconst Host
Pingback: - ECG Oxford
Nicely explained
Pingback: Heat Stroke - Early Warning Signs, Treatment - Modern Health
Pingback: Health Benefits of Tulsi Plant - AcconstHost
Pingback: Natural Remedies for Gastritis (Stomach Ulcers) - MedWebMD