History
A 12-year-old male presents to the clinic with a complaint of dark-colored urine for the past week. His mother reports that he had a sore throat approximately three weeks ago, which was treated symptomatically at home. The patient also mentions a reduction in urine output over the past few days and has felt increasingly tired.
Past Medical History:
- No significant past medical history
- No known allergies
- Up-to-date with vaccinations
Family History:
- No family history of kidney disease
Social History:
- Lives at home with parents
- Attends school regularly, no recent travel history
Examination Findings
On physical examination, the patient appears moderately ill with the following findings:
Vital Signs:
- Temperature: 36.8°C
- Blood Pressure: 150/95 mmHg
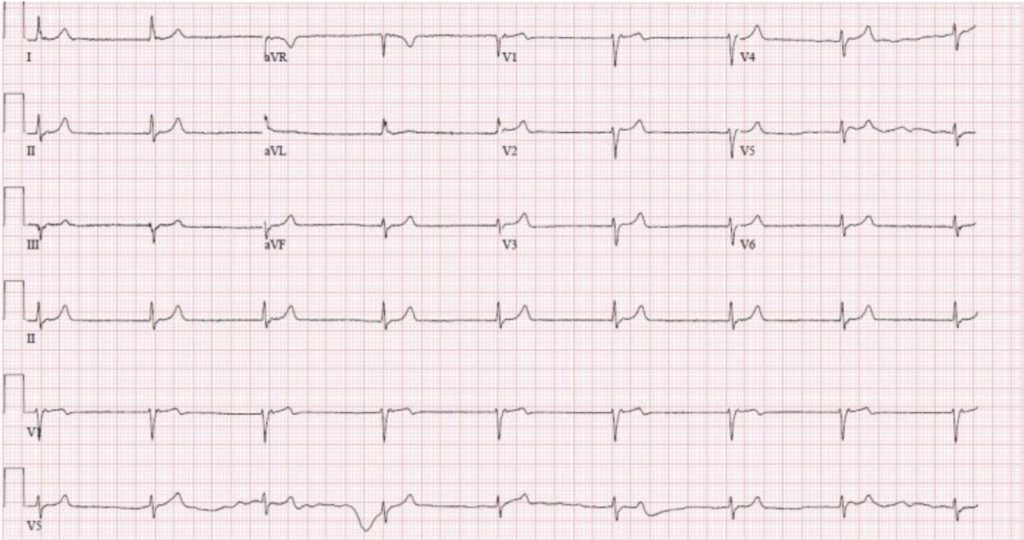
- Heart Rate: 90 bpm
- Respiratory Rate: 18 breaths per minute
General Appearance:
- Periorbital edema
- Mild pitting edema in both lower extremities
Cardiovascular Examination:
- Normal heart sounds, no murmurs
- Elevated jugular venous pressure
Respiratory Examination:
- Clear breath sounds bilaterally
Abdominal Examination:
- No organomegaly
- No tenderness on palpation
Urine Examination:
- Dark-colored urine sample provided
Laboratory Findings
Key laboratory investigations reveal:
Urinalysis:
- Hematuria: Numerous red blood cells (RBCs) per high power field (hpf)
- Red cell casts present
- Proteinuria: 1.5 g/day
Blood Tests:
- Serum Creatinine: 1.8 mg/dL (elevated)
- Blood Urea Nitrogen (BUN): 40 mg/dL (elevated)
- Serum Albumin: 3.5 g/dL (normal to low)
- Anti-streptolysin O (ASO) Titer: Elevated
- Complement C3: Low
- Complete Blood Count (CBC):
- Hemoglobin: 12 g/dL
- White Blood Cells (WBC): 10,000 cells/mm³
- Platelets: 200,000 cells/mm³
Serologic Tests:
- Antinuclear Antibody (ANA): Negative
- Antineutrophil Cytoplasmic Antibodies (ANCA): Negative
- Anti-Glomerular Basement Membrane (Anti-GBM) Antibodies: Negative
Radiology
Renal Ultrasound:
- Kidneys are bilaterally enlarged with increased echogenicity
Diagnosis
Based on the clinical presentation, laboratory findings, and radiologic imaging, the diagnosis of nephritic syndrome, likely secondary to post-streptococcal glomerulonephritis, is made.
Differential Diagnosis
- IgA nephropathy
- Lupus nephritis
- Henoch-Schönlein purpura
- Goodpasture syndrome
- Membranoproliferative glomerulonephritis (MPGN)
Management
Initial Management
- Blood Pressure Control: Antihypertensives (ACE inhibitors or ARBs)
- Fluid Management: Diuretics to manage edema
- Dietary Restrictions: Sodium and fluid restriction
Specific Treatment
- Antibiotics: To eradicate any residual streptococcal infection if present
- Steroids: Considered in severe cases or if rapidly progressive glomerulonephritis is suspected
Follow-Up
- Regular monitoring of renal function, blood pressure, and proteinuria
- Repeat urinalysis and serologic tests as needed
Conclusion
Nephritic syndrome is a potentially serious condition requiring prompt diagnosis and management. Early recognition, appropriate laboratory evaluation, and targeted treatment are essential for optimal patient outcomes. Regular follow-up is necessary to monitor disease progression and prevent complications.