Abstract
Guillain-Barré Syndrome (GBS) is an acute polyradiculoneuropathy presenting with progressive weakness and areflexia. However, its diagnosis can be challenging in cases with atypical history and normal initial nerve conduction studies (NCS). This case study highlights the clinical decision-making process in an 18-year-old female in India, where high GBS prevalence influenced the diagnostic and treatment approach despite inconclusive early investigations.
Case Presentation
Patient Information
- Age & Gender: 18-year-old female
- Presenting Complaint: Progressive weakness in both lower limbs over three days, followed by upper limb involvement
- Medical History: No significant past medical history
- Family & Travel History: No recent illness, vaccination, or gastrointestinal/respiratory infection reported
Clinical Examination
- Bilateral lower limb weakness (proximal > distal)
- Absent deep tendon reflexes
- No sensory loss
- Mild facial weakness but no bulbar or respiratory involvement
- Normal bowel and bladder function
Diagnostic Workup
Initial Investigations
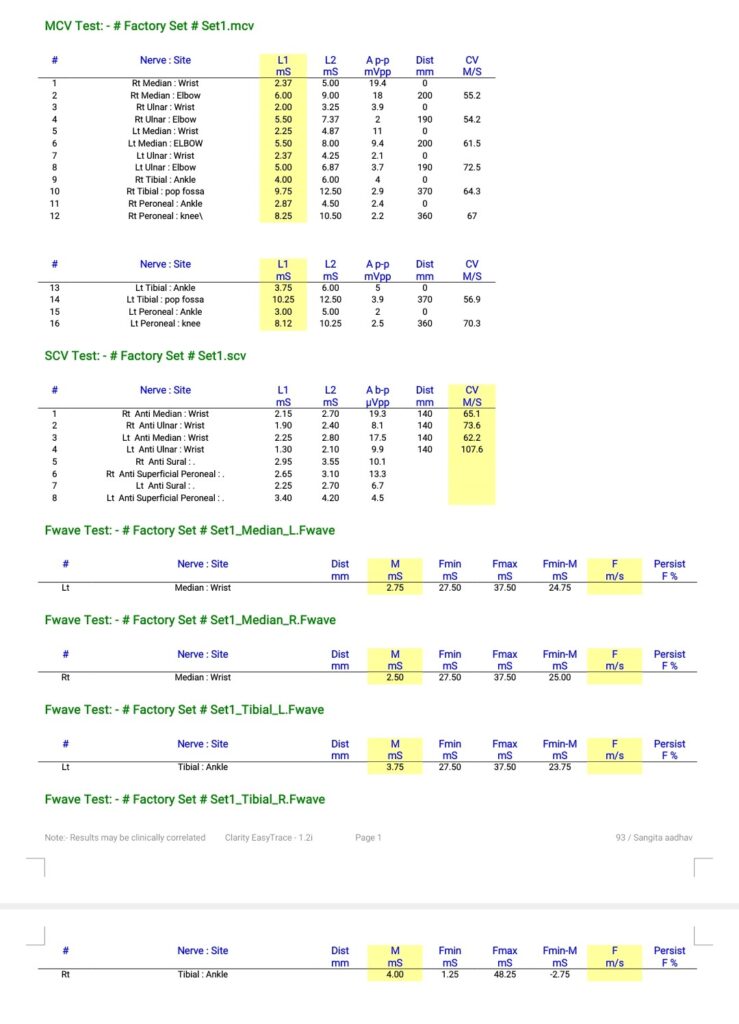
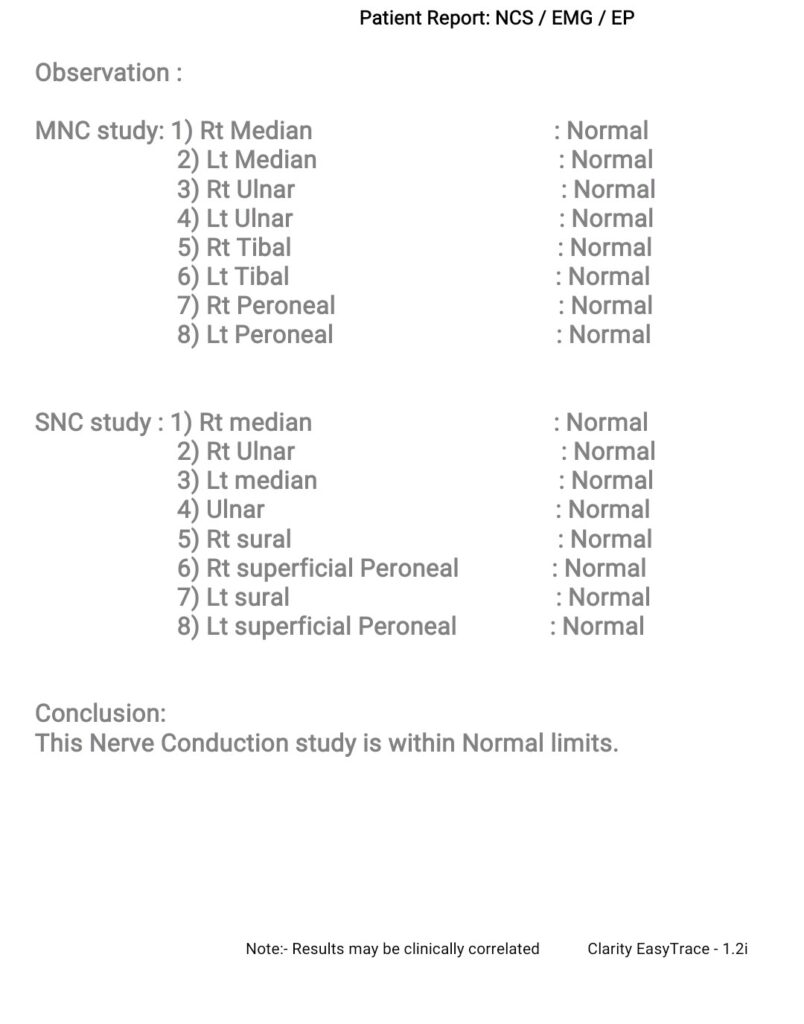
- Nerve Conduction Study (NCS): Normal
- Cerebrospinal Fluid (CSF) Analysis: Normal protein and cell count (lumbar puncture delayed)
- MRI Brain and Spine: No significant abnormalities
- Blood Work: Normal electrolytes, thyroid function, and inflammatory markers
Diagnostic Challenge
Despite the normal NCS, the patient’s progressive weakness and areflexia raised strong clinical suspicion of GBS. Given the high prevalence of GBS in India and the potential for false-negative NCS findings early in the disease course, empirical treatment was initiated.
Management
The patient was treated with:
- Intravenous Immunoglobulin (IVIG) (0.4 g/kg/day for 5 days)
- Supportive care: Physiotherapy, deep vein thrombosis (DVT) prophylaxis, and monitoring for respiratory distress
Clinical Course & Outcome
- By Day 5, mild improvement in limb strength was observed.
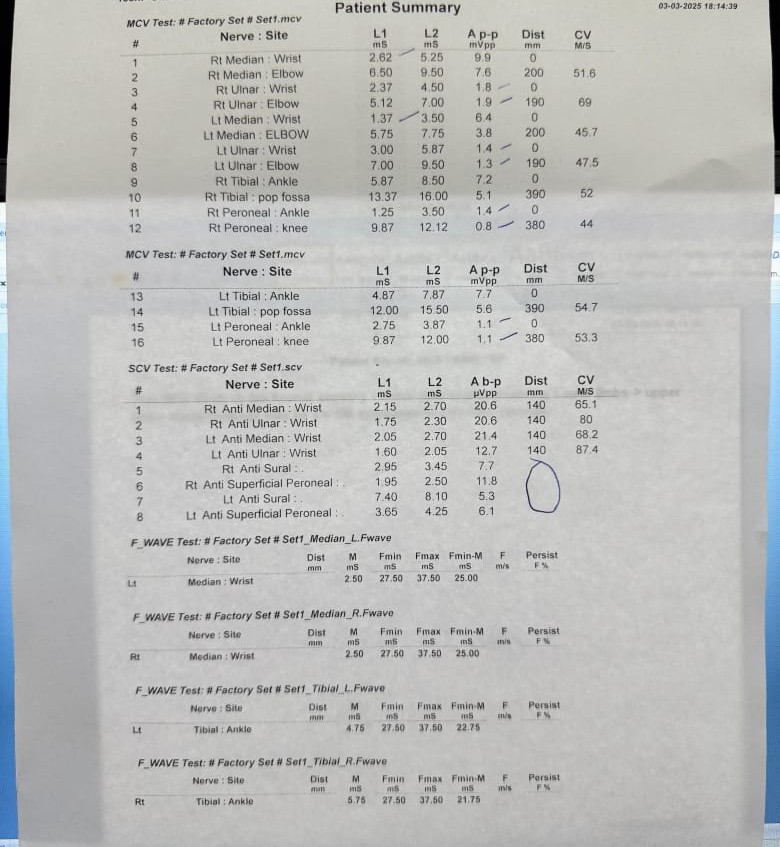
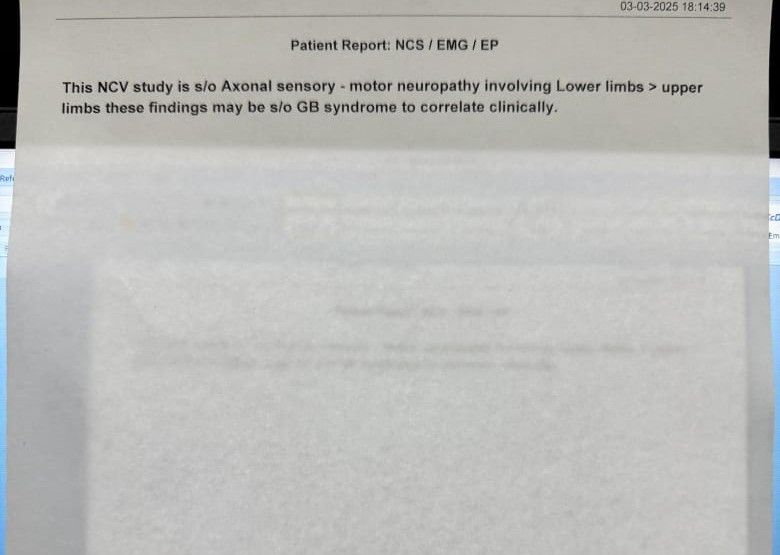
- Repeat NCS in the second week revealed demyelinating features consistent with GBS.
- By Week 2, further recovery was noted, with partial return of deep tendon reflexes.
- The patient was discharged with physiotherapy and followed up at 6 weeks, showing significant motor recovery.
Discussion
GBS Diagnosis Despite Normal Initial NCS
- Early-stage GBS may not always show electrophysiological abnormalities due to subclinical demyelination.
- CSF albuminocytological dissociation may take 1–2 weeks to appear, making early lumbar puncture non-contributory.
- High clinical suspicion and prevalence of GBS in India influenced the decision to treat empirically, preventing complications.
Lessons Learned
- NCS findings in early GBS may be misleading, and repeat studies are essential.
- Timely treatment with IVIG/plasmapheresis is crucial, even in diagnostically uncertain cases.
- GBS should remain a primary consideration in acute flaccid paralysis, especially in endemic regions.
NCS study at presentation:
Ncs Study in second week
Conclusion
This case underscores the importance of clinical judgment in diagnosing and managing GBS, particularly in regions with high disease prevalence. Repeat NCS in the second week confirmed the diagnosis, reinforcing the need for serial electrophysiological studies when initial tests are inconclusive. Early treatment, even in the absence of definitive initial tests, can significantly impact patient outcomes.
