Case Presentation
A 52-year-old male presented to the emergency department with complaints of progressive shortness of breath over one week, chest discomfort, and lightheadedness. He reported difficulty lying flat and increased fatigue. Past medical history was significant for hypertension and chronic kidney disease.
On examination, the patient was anxious, with a blood pressure of 90/60 mmHg, heart rate of 120/min, and respiratory rate of 24/min. Jugular venous distension was noted. Heart sounds were muffled, and peripheral pulses were weak. ECG showed low voltage QRS complexes and electrical alternans. Bedside echocardiography revealed a large pericardial effusion with diastolic collapse of the right atrium, suggestive of cardiac tamponade.
Emergency pericardiocentesis was performed, draining 500 ml of sero sanguinous fluid. The patient’s hemodynamics improved immediately.
Introduction
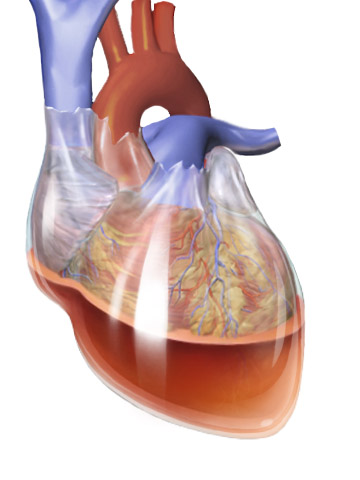
Cardiac tamponade is a life-threatening condition where fluid accumulates in the pericardial sac, leading to increased intra pericardial pressure. This pressure compresses the heart chambers, especially during diastole, impairing ventricular filling and reducing cardiac output. If untreated, it can lead to circulatory collapse and death.
Causes
Cardiac tamponade may result from a wide range of conditions:
- Trauma – Penetrating chest injury or blunt trauma.
- Malignancy – Lung, breast cancer, or metastatic tumors invading the pericardium.
- Infections – Tuberculosis, viral pericarditis.
- Uremia – Seen in advanced chronic kidney disease.
- Autoimmune diseases – Lupus, rheumatoid arthritis.
- Post-cardiac surgery or post-MI (Dressler’s syndrome).
- Anticoagulation – Spontaneous bleeding into the pericardial space.
- Aortic dissection – With rupture into the pericardium.
Signs and Symptoms
Typical features include:
- Dyspnea, orthopnea
- Chest discomfort
- Hypotension
- Tachycardia
- Pulsus paradoxus (drop in systolic BP >10 mmHg during inspiration)
- Muffled heart sounds
- Elevated jugular venous pressure (JVP)
- Weak peripheral pulses
- Altered mental status in severe cases
Beck’s Triad: Hypotension, muffled heart sounds, raised JVP.
Clinical Examination
- Tachycardia and hypotension
- Raised JVP with prominent x descent and absent y descent
- Pulsus paradoxus (can be measured with a sphygmomanometer)
- Diminished heart sounds on auscultation
- Hepatomegaly (in chronic cases)
Investigations
- Electrocardiogram (ECG):
- Low voltage QRS complexes
- Electrical alternans (variation in QRS amplitude)
- Chest X-ray:
- Enlarged, globular (“water bottle”) shaped cardiac silhouette in large effusion
- Echocardiography (diagnostic modality of choice):
- Pericardial effusion
- Right atrial or right ventricular diastolic collapse
- Swinging heart motion
- Dilated IVC with poor respiratory variation
- CT/MRI:
- Helpful in complex or loculated effusions
- Pericardial fluid analysis:
- To determine etiology (infection, malignancy, TB)
Interventions and Management
Emergency intervention is crucial.
- Pericardiocentesis:
- First-line emergency treatment
- Can be guided by echocardiography or fluoroscopy
- Needle inserted into pericardial space (usually subxiphoid approach)
- Immediate relief of symptoms and improvement in hemodynamics
- Pericardial window or surgical drainage:
- For recurrent or loculated effusions
- Performed via thoracotomy or video-assisted thoracoscopic surgery (VATS)
- Intravenous fluids:
- Temporarily maintain preload and cardiac output
- Treat underlying cause:
- Anti-tubercular therapy, antibiotics, cancer management, etc.
Complications
- Cardiogenic shock
- Arrhythmias
- Recurrence of effusion
- Pericardial constriction
- Death if untreated
Follow-up
- Serial echocardiography
- Monitoring of pericardial drain if left in place
- Repeat fluid analysis in recurrent cases
- Treatment of underlying condition
Differential Diagnoses (DDs)
- Constrictive pericarditis
- Severe heart failure
- Tension pneumothorax
- Massive pulmonary embolism
- Acute MI with cardiogenic shock
Newer Modalities and Advances
- Point-of-care ultrasound (POCUS): Allows early bedside diagnosis by emergency physicians.
- Echocardiographic contrast agents: Better delineation of loculated effusions.
- Pericardioscopy: Minimally invasive approach to visualize and biopsy pericardium.
- Molecular diagnostics: PCR for TB and oncogene testing for malignant pericardial fluid.
